ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Aortic Translocation for TGA with VSD and PS
Index
Editor Note
Patient Selection
This procedure was introduced for the management of patients with complex transposition of the great arteries (TGA) with a ventricular septal defect (VSD) and pulmonary stenosis (PS). The technique has proven especially useful in the subset of patients with anatomic variables that complicate the performance of a Rastelli repair, which include: an inlet or restrictive VSD, a small right ventricle, a straddling atrioventricular valve and anomalous coronary anatomy (preventing a distal right ventriculotomy). This procedure could also be applied to patients with a double outlet right ventricle with malposition of the great arteries and PS.
Operative Steps
Cardiopulmonary Bypass
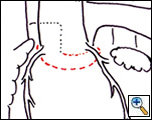
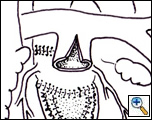
A standard median sternotomy is performed followed by initiation of cardiopulmonary bypass with bicaval cannulation. Under moderate hypothermia (28 degrees Centigrade) the proximal coronary arteries are mobilized and the aortic root is harvested from the right ventricle (RV) (Figure 1, left). Alternatively, cardioplegic arrest can be instituted and the coronary artery buttons harvested from the aorta before proceeding with the mobilization of the aortic root.
Operative Approach
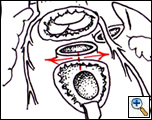
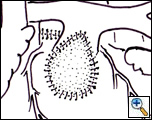
The pulmonary artery is transected proximally, the pulmonary valve is resected and the conal septum divided (Figure 1, right). The aortic root is then translocated posteriorly and sutured to the pulmonary valve annulus posteriorly (Figure 2, left) and to the crest of the VSD (or the VSD patch) anteriorly (Figure 2, right). The coronary arteries, if detached, are then reimplanted.
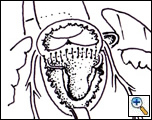
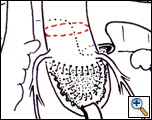
The ascending aorta is transected and a small section removed in order to prevent bowing of the ascending aorta which will result in posterior compression of the pulmonary arteries. The Lecompte maneuver is then performed (Figure 3, left) followed by the ascending aorta anastomosis. Right ventricle to pulmonary artery continuity is established by direct anastomosis (Figure 3, right; Figure 4) or with a conduit.
Preference Card
- Patch material for the VSD closure
- Glutaraldehyde to soak the autologous pericardial patch utilized to reconstruct the right ventricular outflow tract (anterior patch)
- Transesophageal echocardiography
Tips & Pitfalls
- Extensive mobilization of the coronary arteries is important to prevent kinking or torsion during translocation.
- If needed, consider detaching just one or both coronary arteries during translocation. After translocation the coronary arteries may need to be reimplanted at a different site in the aorta (not at the harvest site).
- If the coronary arteries and aortic root are harvested “en bloc”, it can be done with a beating heart. This allows you to detect the presence of coronary ischemia (EKG changes) or aortic insufficiency during translocation.
- When suturing the translocated aortic root be careful not to create any distortion which could result in the eventual development of aortic insufficiency.
- The main pulmonary artery is usually hypoplastic; thus when a direct connection between the right ventricle and the PA is being performed we would augment the anterior wall of the main PA with autologous pericardium.
- At times the outflow of the RV needs to be enlarged
Results
The overall experience with aortic translocation is somewhat limited and there are just a few reports in the medical literature. In our initial experience with 12 patients who underwent aortic translocation there was one early death (8.3%). At a median follow-up of 33 months all patients where alive, ten had normal ventricular function and three had developed moderate aortic insufficiency. Nikaidoh reported excellent results in a series of 17 patients undergoing aortic translocation with one early death and no late mortality with a mean follow-up period of 11.4 years. None of the patients developed significant aortic insufficiency.
References
- Morell VO, Jacobs JP, Quintessenza JA. Aortic translocation and biventricular outflow tract reconstruction in the management of complex transposition of the great arteries with ventricular septal defect and pulmonary stenosis: results and follow-up. Ann Thorac Surg 2005;79:2089-93.
- Morell VO, Jacobs JP, Quintessenza JA. Surgical management of transposition with ventricular septal defect and obstruction to the left ventricular outflow tract. Cardiol Young 2005;15(Suppl 1):102-5.
- Morell VO, Jacobs JP, Quintessenza JA. The role of aortic translocation in the management of complex transposition of the great arteries. Semin Thorac Surg Pediatr Card Surg Annu 2004;7:80-4.
- Nikaidoh H. Aortic translocation and biventricular outflow tract reconstruction : a new surgical repair for transposition of the great arteries associated with a ventricular septal defect and pulmonary stenosis. J Thorac Cardiovasc Surg 1984;88:365-72.
- Yeh T, Ramaciotti C, Leonard SR, Nikaidoh H. Superior preservation of the left ventricular outlet after the aortic translocation (Nikaidoh) procedure. Presented at the Fourth World Congress of Pediatric Cardiology and Cardiac Surgery, 2005.