ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
The Microdebrider Allows for Rapid Removal of Obstructing Airway Lesions
Obstruction of the central airways may develop in 30-40% of all patients with lung cancer and is being increasingly diagnosed in patients with benign disorders such as post intubation tracheal stenosis and connective tissue diseases.
Introduction
Obstruction of the central airways may develop in 30-40% of all patients with lung cancer and is being increasingly diagnosed in patients with benign disorders such as post intubation tracheal stenosis and connective tissue diseases [1]. Endoscopic palliation is often necessary in order to relieve symptoms of dyspnea, establish a diagnosis, and serve as a bridge to other therapies such as surgical resection and reconstruction. Until recently, the technique of dilation and curettage with a rigid bronchoscope, pioneered by Gustav Killian and Chevalier Jackson in the last century, were the mainstay of endoscopic therapy [2]. Interventional bronchoscopists now have more tools at their disposal including airway balloons, argon plasma coagulation, laser, electrocautery, and a new tool - the microdebrider.
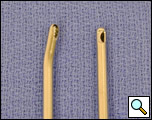
The microdebrider (Xomed, Jacksonville, FL) is a three component instrument. First, the disposable blade is a hollow metal tube coupled to suction that cuts obstructing tissue and simultaneously removes it from the airway (Figure 1). Second, the hand piece drives the blade via an electrically powered motor and is compatible with blades of various sizes and configurations. Regular wall suction tubing connects to the hand piece to provide suction to the blade (Figure 2). Third, the console controls the hand piece via a foot pedal and allows the operator to select the speed and the direction of rotation of the blade (Figure 3).

Figure 2. The handpiece enables spatial control of the blade and is attached to suction to evacuate debrided materials.

Figure 3. The control console permits the operator to select blade speed and direction with use of foot switches.
Figure 1. Two of the various types of blades are evident in the working end of the microdebrider.
Figure 2. The handpiece enables spatial control of the blade and is attached to suction to evacuate debrided materials.Figure 3. The control console permits the operator to select blade speed and direction with use of foot switches.
Technique
While various airway blades are available, we favor an angled tip tracheal blade with a serrated edge. The slight angle to the tip of the blade allows for excellent maneuverability in the airway with the ability to reach most lesions in the trachea and proximal portions of the mainstem bronchi. We prefer the serrated blades to smooth blades, as we have found them superior for cutting redundant tissue and pulling the tissue into the orifice of the blade so that it may be suctioned out of the field. Finally, when setting up the console for the direction of blade rotation, we employ an oscillating mode rather than a forward or reverse mode. An oscillating blade is less likely to become clogged with tissue. In terms of blade speed, we prefer slower speeds in the range of 1,000 to 2,000 rpm as they allow more time for tissue to be drawn up into the aperture of the blade and result in rapid debridement [3].
Microdebrider blades currently available have diameters that range from 5-7mm and are thus too large to fit down the instrument channel of a flexible scope. They are also rigid, further limiting application with a flexible scope. Therefore, they must be employed with either a rigid bronchoscope or a suspension laryngoscope. An operating video telescope is placed into the airway in tandem with the microdebrider so that tissue dissection may be carried out with optimal visualization and control.
The video demonstrates the microdebrider in action in the case of a 60 year old man with obstruction of the distal trachea and right mainstem bronchus due to non-small cell carcinoma.
Video 1
We have developed the following tenets of proper dissection with the microdebrider:
- Position the distal end of the telescope approximately 10-15mm from the field of dissection. This allows for improved depth perception while minimizing the risk of soiling the lens with blood or debris.
- Employ suction to bring the tissue into the aperture of the blade. This allows the operator to selectively target tissue to remove and helps avoid inadvertent dissection of normal airway tissue.
- Position the telescope so that the blade aperture is always visible during dissection. A general principle of any surgical technique, keeping a close eye on the business end of the instrument prevents mishaps.
- Never direct the blade aperture toward the posterior membranous portion of the trachea or bronchus when dissecting lesions in this vicinity. The membranous airway is the least rigid structure and represents a danger zone for possible airway perforation and fistulization.
- Employ the rigidity of the blade to your advantage. With the blade inactive, probe the airway with the blunt tip of the instrument to give you a tactile feel of the airway wall and the field of dissection.
- Have thermal modalities present in order to control bleeding that is not responsive to tamponade with the rigid scope.
Discussion
This new generation airway tool has its roots in the rotary vacuum shaver introduced in 1968 by Urban to assist in removal of acoustic neuromas. After considerable evolution and improvements in design, present day microdebriders are employed by a variety of specialists from orthopedic surgeons to otolaryngologists. The microdebrider is not only useful for endoscopic dissection of obstructing airway tissue, but it is employed in a variety of applications including endoscopic sinus surgery, cosmetic surgery, and endoscopic joint surgeries [4].
Simoni et al were the first to report use of the microdebrider as first line therapy to remove obstructive malignant tissue in the airway [5]. Twenty seven patients with advanced laryngotracheal carcinoma underwent endoscopic debridement with the microdebrider followed by radiation therapy. All patients had relief of dyspnea and only three patients eventually required tracheotomy: one due to vocal cord paralysis and two due to radiation induced laryngotracheal edema. These authors found the microdebrider to be a safe, quick, and effective tool in their patients.
We have reported our experience with removing both benign and malignant airway lesions with the microdebrider [3,6,7]. We employed the microdebrider in 44 patients with central airway obstruction due to various causes: granulation tissue from tracheotomy or prior intubation – 24 ;, idiopathic subglottic stenosis – 4; stent-related granulation tissue – 4; granulation tissue after surgical airway reconstruction – 1; airway papilloma – 1; non-small cell carcinoma – 8; small cell carcinoma – 1; and thyroid carcinoma - 1. Obstructing lesions were removed rapidly with a range of dissection times from 2 to 20 minutes. Despite some of the lesions being malignant, there were no episodes of significant airway bleeding and no other procedure-related complications. All patients had relief of dyspnea postoperatively.
While other modalities, including laser-assisted rigid debridement, are available for removing obstructive tissue from the central airways, the microdebrider has important advantages. First, all thermal modalities require that the operator debride, suction, and apply thermal energy to the airway in a sequential manner. In the case of laser, electrocautery, and argon plasma coagulation, care must be taken to deplete airway oxygen levels before thermal energy is delivered in order to avoid airway fires. This may mean that some interventions are quite prolonged. In contrast, the microdebrider combines suction and dissection and may obviate the need for thermal modalities altogether, thus shortening intervention times. Second, the simultaneous removal of blood and debris by the microdebrider allows for greater visualization of airway lesions during dissection as compared to traditional rigid techniques. Third, the ability of the microdebrider to draw tissue into the blade aperture allows for the surgeon to precisely limit its effects. Injury to normal airway mucosa can be avoided and serious consequences of rigid debridement such as airway perforation, injury to vessels, and fistula formation can be avoided.
An important caveat is that investigators have reported that microdebriders have been associated with inadvertent resection of normal tissue during sinus surgery[8]. While this complication usually occurs with the use of a drilling bur, it also may occur with cutting blades. Factors associated with such misadventures include: 1) overzealous suction pressure applied to the hand piece resulting in excess tissue being drawn into the blade, and 2) inadequate visualization of the blade or bur.
Conclusion
The microdebrider represents a new generation airway tool that allows for safe, rapid, and effective removal of obstructing tissue from the central airway. The technology is readily compatible with the rigid bronchoscopes already stocked by most thoracic operating theaters. Used properly, the microdebrider allows for greater preservation of normal airway mucosa than traditional endoscopic techniques.
References
- Ernst A, Feller-Kopman D, Becker HD, et al. Central airway obstruction. Am J Respir Crit Care Med 2004;169:1278-1297.
- Mathisen DJ, Grillo HC. Endoscopic relief of malignant airway obstruction. Ann Thorac Surg 1989;48:469-473.
- Lunn W, Garland R, Ashiku S, et al. Microdebrider bronchoscopy: a new tool for the interventional bronchoscopist. Ann Thorac Surg 2005;80:1485-1488.
- Powered Instrumentation in Otolaryngology-Head and Neck Surgery. 1 ed. San Diego: Singular, 2001
- Simoni P, Peters GE, Magnuson JS, et al. Use of the endoscopic microdebrider in the management of airway obstruction from laryngotracheal carcinoma. Ann Otol Rhinol Laryngol 2003;112:11-13.
- Lunn W, Gunter E, Garb H, et al. Use of a microdebrider for management of intubation related laryngotracheal granulation tissue. Am J Respir Crit Care Med 2003;150:A526.
- Lunn W, Loebe M, Bechara R, et al. Further Experience with Microdebrider Bronchoscopy: A New Tool for Treating Central Airway Obstruction. Chest 2005;128:209S.
- Kuhnel T, Hosemann W, Rothammer R. Evaluation of powered instrumentation in out-patient revisional sinus surgery. Rhinology 2001;39:215-219.