ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
New Technological Approach to Pulmonary Nodulectomy
Patient Selection

|
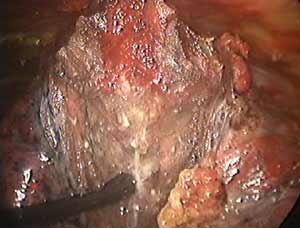
When an isolated pulmonary nodule is lying deep to a flat surface of the lung, VATS wedge resection using the conventional endoscopic staple-cutter is often technically difficult. Even if this could be done, it usually sacrifices more functional lung tissue than would be necessary or desirable. This could have a major impact on the recovery of patients who are elderly, frail with multiple co-morbidities, and borderline lung function. It is for this group of patients that new technological approaches may offer an advantage. Patients with peripheral pulmonary nodules for diagnostic or therapeutic wedge resection are suitable candidates to consider. The nodule should ideally be located in the peripheral one-third of the lung, and should be less than 3cm in maximal diameter (Figure 1).
Operative Steps
The new technology is incorporated in an instrument (TissueLink, Dover, NH) that provides a continuous flow of electrically conductive saline to the interface between a metal electrode and tissue. The saline couples radiofrequency electrical energy into tissue where it is converted into thermal energy. The flow of saline provides cooling to limit peak tissue temperatures to 100° C or less. Tissue temperatures from conventional electrosurgical devices can easily exceed 300° C, resulting in tissue desiccation, char formation, smoke generation, electrodes sticking to tissue, and undesired lateral thermal damage. The new technology avoids these undesirable tissue effects, while producing the levels of tissue temperature required to achieve both hemostasis and pneumostasis of lung tissue. The use of saline in combination with radiofrequency electrical energy has also been applied to other clinical areas, such as interstitial tumor ablation in the kidney1 and liver2, as well as to cardiac3 and prostate ablation4.

|
The TissueLink device comes in two sizes (the endoscopic version being longer) and is primed with saline solution from an infusion pump (Figure 2). The device is equipped with a floating ball electrode tip. There is an on/off radiofrequency activation switch (used in conjunction with a conventional electrosurgical generator) on the hand piece, and saline and electrical lines exit at its end.
The patient is placed in a full lateral decubitus position under a general anesthetic, and is prepped and draped as for a full thoracotomy. Selective one lung ventilation is used. A three-port VATS technique is preferred5.
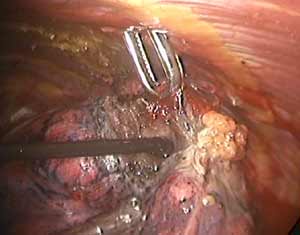
The TissueLink device does not perforate or cut into tissue (in contrast to conventional electrocautery). Instead, the surface of the tissue is painted with the device, which first coagulates and then shrinks the lung tissue (Figure 3). The surgeon then divides the coagulated tissue with scissors (Figure 4). Compared with conventional electrocautery, the TissueLink device usually leaves the resection bed more hemostatic and pneumostatic.
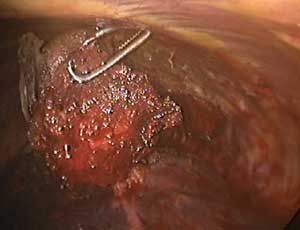
Slightly longer time is needed for resection using the TissueLink device. It is excellent in sealing small (1mm or less) bronchioles in the resection bed. The floating ball device should be applied directly over the bronchiole for one to two minutes to accomplish this. The TissueLink device, by nature of the technology, generates less smoke than conventional electrocautery. However, a small amount of steam is inevitable, and it is advisable to keep a sucker (a conventional Yankauer sucker works best) close to the surgical field, which also may be used to exert counter-traction on the lung tissue to facilitate dissection (Figure 5). As with all potential cancers, specimens should be placed in a bag before they are removed through a port site (Figure 6).
Preference Card
The author prefers to use conventional thoracic instruments for all his VATS cases. Sponge holding forceps are universally available and excellent in handling the lung. A thoracotomy tray should be at hand. A conventional electrocautery generator is necessary for use in conjunction with the TissueLink device.
Tips & Pitfalls
- There is a steep learning curve associated with use of the device. Provide extra time for the first few cases.
- The device does not vaporize or divide tissue. Once coagulated, tissue must be divided with scissors.
- Use of conventional suction will help evacuate steam generated by the device.
- Frequent palpation of the area of interest will assist in selecting the boundaries of resection and minimize excision of excess tissue.
- There should not be any arcing between the electrode and tissue. If this occurs, it suggests that the flow of saline has been interrupted. This should be adjusted before proceeding further
Results
With the advent of VATS, peripheral lung nodules can often be approached using mechanical staplers for resection, which has become the resection approach of choice for many centers. However, for larger nodules (over 2cm) and especially those lying deep to a flat lung surface, wedge resection using this technique is often difficult, even hazardous.
A solution was offered over twenty years ago by the Russian surgeon, Mikhail Perelman using electrocautery to achieve precise, non-anatomical lung resection, a technique which was subsequently popularized by Joel Cooper6. This precision cautery excision, as it is often referred to, is not ideally suitable for the VATS approach, however. The technique requires that the lung be in an inflated state. Because the electrocautery is often required to be turned up to a high setting, there is moderate amount of smoke generation, and charred tissue sticking to the electrode demanding frequent cleaning. Finally, because the electrode can perforate a moderate-sized blood vessel (3mm diameter and larger) before it gets coagulated, bleeding could be troublesome and difficult to control thoracoscopically.
Landreneau and colleagues more recently advocated the use of Nd:YAG laser, either alone or in combination with mechanical stapler, to approach difficult non-anatomical resections using VATS7. The advantage of laser appears to be its ability to achieve better hemostasis compared to electrocautery. However, the high initial cost for set up, coupled with the stringent safety requirements have deterred many surgeons from using this.
The TissueLink device has the ability to achieve good hemostasis (as it does not perforate vessels) without the high initial cost. Like other new techniques and technology, there is an initial steep learning curve for the surgeon. As the surgeon is required to individually divide the coagulated vessels and bronchioles, more time has to be allowed for this procedure compared to when conventional electrocautery is used. Also, as the operated lung is deflated, there is a tendency that the surgeon could remove more functional lung tissue than would be necessary or desirable. However, this can be overcome by experience.
We have used the TissueLink floating-ball device on ten patients (five males, mean age 56.4 years) with peripheral lung nodules (diameter 1.5 ± 0.7 cm) for diagnostic or therapeutic wedge resections. There has been no mortality or intraoperative complication. The mean operation time was 76 mins (range 38 - 122). Average chest drain duration was 3.4 days (range 1 to 10) and postoperative hospital stay was 5 days (range 2 to 12). One patient had postoperative persistent airleak that resolved on its own. The thermal spread on the resected specimen averaged 2.5 mm (range 2.2 - 3.6). There has been no late complication after an average follow up of 9 months.
VATS nodulectomy using this device appears technically feasible and safe, and has several advantages over conventional electrocautery. Its exact role in thoracic surgery, however, needs to be defined by prospective studies comparing this technique with conventional approaches. Nonetheless, it seems appropriate that this device should be in the armamentarium of the thoracic surgeon.
Disclosure Statement
Anthony P.C. Yim, MD, is a member of the Physician Advisory Board of TissueLink Medical, Inc.
References
- Patel VP, Leveille RJ, Hoey MF et al. Radiofrequency ablation of rabbit kidney using liquid electrode: acute and chronic observations. J Endourol 2000;14:155-159.
- Miao Y, Ni Y, Mulier S, Wang K, Hoey MF et al. Ex vivo experiment on radiofrequency liver ablation with saline infusion through a screw-tip cannulated electrode. J Surg Res 1997; 71:19-24.
- Liem LB, Pomeranz M et al. Electrophysiological correlates of transmural linear ablation. PACE 2000; 23:40-46.
- Hoey MF, Dixon CM and Paul S. Transurethral prostate ablation using saline-liquid electrode introduced via flexible cystoscope. J Endourol 1998;12:461-468.
- Lin JC, Landreneau RJ. Strategic planning for video-assisted thoracic surgery. In Yim APC, Hazelrigg SR, Izzat MB et al (eds): Minimal Access Cardiothoracic Surgery. Philadelphia. W.B. Saunders, 2000, p 28-36.
- Cooper JD, Perelman M, Todd TR, et al. Precision cautery excision of pulmonary lesions. Ann Thorac Surg 1986;41:51-53. [View abstract]
- Landreneau RJ, Keenan RJ, Hazelrigg SR, et al. VATS wedge resection of the lung using the neodymium: yttrium-aluminium garnet laser. Ann Thorac Surg 1993;56:758-761. [View abstract]