ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Single-Incision VATS Right Upper Lobe Posterior Segmentectomy
A 62-year-old man with a history of arterial hypertension, diabetes mellitus, and prior smoking underwent a sigmoidectomy in 2011 for an adenocarcinoma, and received adjuvant chemotherapy. In 2013, after 24 months of follow-up, bilateral pulmonary nodules and mediastinal lymph nodes appeared. The first biopsy was negative. In 2014, a new fine-needle biopsy showed pulmonary metastases. Chemotherapy plus antiangiogenic treatments were administered. With no evidence of disease progression and two PET positive residual pulmonary nodules in the right-upper and left-lower lobes, surgery for both nodules was indicated.
As the RUL was initially accessible for a wedge resection, the LLL nodule was approached first. A non-intubated SI-VATS S6 LLL anatomical segmentectomy was performed in April 2016. Four months later, a segmental S6 bronchopleural fistula was diagnosed and successfully managed with an endobronchial valve. A new chest scan then showed growth of the RUL lesion, requiring a posterior S2 segmentectomy instead of the initial wedge planned (Figure 1).
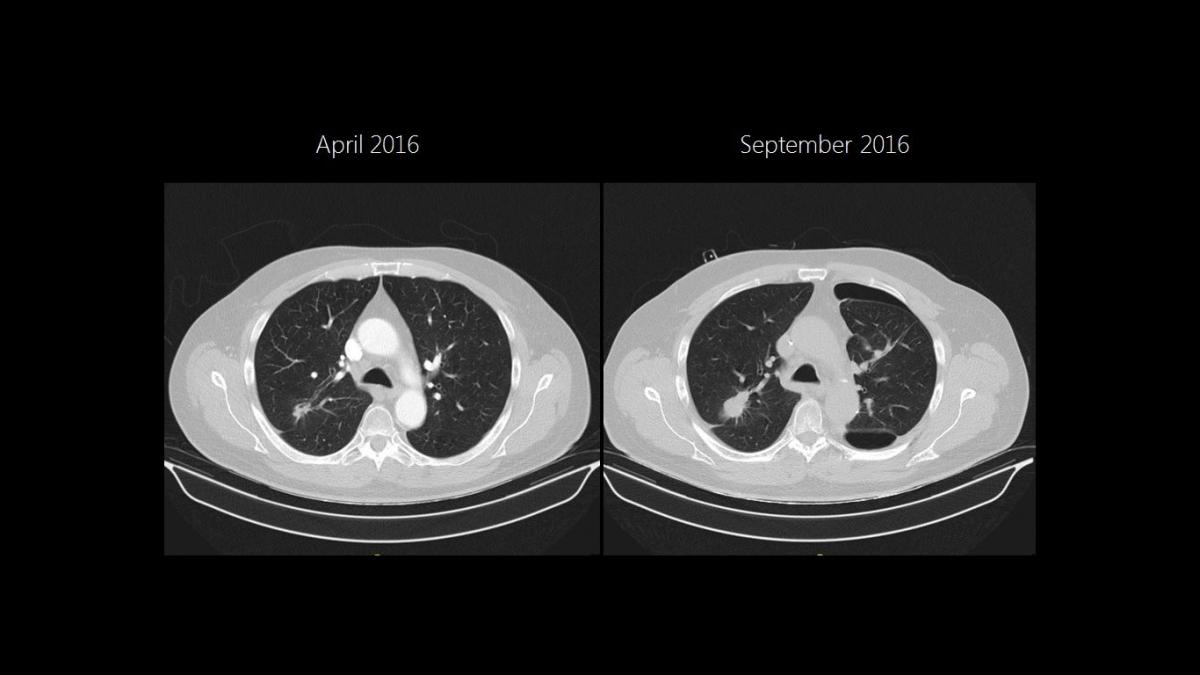
Figure 1
A posterior segmentectomy was performed through a 4 cm incision placed in the 5th right intercostal space, involving intercostal blocks with bupivacaine of the 3rd to 7th intercostal spaces, as shown in the video.
There was no postoperative air leak, and the right chest tube was removed 48 hours after the surgery. The patient’s pain visual analogue scale scores were 3 and 2 at 24 and 48 hours after surgery. A contralateral empyema in the middle posterior pleural space due to bronchopleural fistula and the valve placement was diagnosed postoperatively. It was successfully managed with wide-spectrum antibiotic therapy and ultrasound-guided drainage. The patient was discharged on the 8th postoperative day with satisfactory chest X-ray (Figure 2). The final pathology report demonstrated a 2 cm intestinal metastasis with free bronchial, vascular, and fissural margins. The patient continues follow-up with medical oncology.

Figure 2
Anatomical segmentectomies are indicated for early stage primary adenocarcinomas, as well pulmonary metastasis and benign conditions. These lung-sparing resections are especially useful in metastatic disease as they preserve healthier parenchyma and functional reserve. This enables future resections in the event of new metastasis development and avoids a pulmonary lobectomy. Experience and anatomical knowledge are mandatory for these procedures in order to avoid complications. Single-incision VATS is a safe approach for these surgeries, as proved in many published series and illustrated in this video.




Comments