ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Thoracoscopic Pericardial Window
Patient Selection
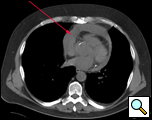 |
| Figure 1. CT scan showing pericardial effusion. |
Hemodynamically stable patients with an undiagnosed pericardial effusion are well suited for a thoracoscopic window. When pericardial, pleural, or pulmonary pathology co-exist and require diagnosis or therapy, a thoracoscopic approach is ideal. If a large piece of pericardial tissue is needed for culture or pathological examination, thoracoscopy provides good exposure and allows for an adequate specimen to be sampled [1]. Known benign effusions that re-accumulate after aspiration should be treated with a thoracoscopic window. Drainage of a purulent pericardial effusion, and early fungal or tuberculous pericarditis where resection of the pericardium to prevent future pericardial constriction is required, are also indications. In patients with descending mediastinitis a window or resection of the pericardium may be warranted as part of the mediastinal debridement. Loculated effusions situated unilaterally or posteriorly are more easily approached thoracoscopically (Figure 1).
Chylopericardium requires a thoracoscopic window and ligation of the thoracic duct [2]. Delayed (3 weeks) hemopericardium or effusions after cardiac surgery are better drained thoracoscopically as are effusions occurring in patients with a remote history of sternotomy [3]. An unusual indication is an effusion in a patient with a substernal gastric or colonic conduit where a subxiphoid approach is not possible.
The side from which to approach the effusion is controversial with advocates for both sides making valid arguments for each. A right sided approach provides more room within the chest to maneuver instruments, for providing exposure, and the phrenic nerve courses just anterior to the hilum of the lung and away from the area of the pericardium to be resected (Video 1). A left sided approach provides a greater surface area of pericardium to work with but, with the phrenic nerve running across the middle of the pericardium, greater care must be taken to avoid nerve injury (Video 2).
The presence of associated pulmonary or pleural pathology to be investigated and the likely presence of pleural adhesions should be taken into account when the side of the approach is to be decided.
A CT scan provides information as to the location and size of the effusion, whether there are loculations, the nature of the parietal pericardium, and associated pulmonary or pleural pathology. Echocardiography provides a dynamic assessment of the physiologic impact of the effusion on myocardial function which helps determine if the patient will be hemodynamically stable to undergo a thoracoscopic pericardial window (Echo 1).
Pericardiocentesis should be attempted prior to the procedure as the information obtained may make it unnecessary or stabilize the patient so that they can undergo a more definitive drainage by thoracoscopy.
Patients with cardiac tamponade and hemopericardium from penetrating trauma until recently were thought not to be suitable for thoracoscopy, but a recently reported series has demonstrated otherwise[5]. A known malignant effusion (other than breast carcinoma or lymphoma) and an inability to tolerate one lung anesthesia are absolute contraindications for this approach. In patients with lymphoma or breast carcinoma, in whom effective systemic therapy may result in prolonged survival, a thoracoscopic approach may be considered. Pleural symphysis is a relative contraindication for a thoracoscopic window being performed through that hemithorax. Patients with chronic constrictive pericarditis should be resected using an open technique and not thoracoscopically.
Operative Steps
General anaesthesia with single lung ventilation is required. Arterial and central venous pressure monitoring may be needed intraoperatively as well as in the postoperative period to guide hemodynamic management. External defibrillator pads are applied to the chest and back before prepping and connected to a defibrillator in case an arrhythmia develops during surgery. The patient is placed in a posterolateral thoracotomy position leaning backwards to allow increased exposure of the pericardium (Figure 2). If there is doubt about the hemodynamic stability of the patient or the ability to tolerate one lung anesthesia, the patient can be placed supine and the side to be approached elevated with a pressure bag or jelly roll to allow access to that side of the chest (Figure 3). In this situation, if the patient becomes unstable, a quick conversion to a subxiphoid window can be performed without having to reposition the patient.
 |
 |
| Figure 2. Patient in a lateral position | Figure 3. Patient position in a semilateral position. |
Epidural anesthesia is not required and intercostal nerve blocks are given as the incisions are made.
 |
| Figure 4. Port placement |
The thoracoscope is introduced in the 7th intercostal space in the midaxillary line or in line with the anterior superior iliac spine on the right. On the left the incision is placed just posterior to this line. The working incision is placed in the posterior axillary line in the 5th intercostal space and is between three and five centimeters in length (Figure 4; Video 3). The intercostal muscles are divided for a distance greater than this and a Weitlaner retractor is used to keep the soft tissue open. This allows for two to three instruments to be simultaneously placed into the chest through one incision. The surgeon stands behind the patient and the table is rolled posteriorly to increase the exposure to the lateral pericardial surface.
With the lung collapsed the phrenic nerve is identified running vertically down along the pericardium and should be visualized throughout the operation. On the left the nerve runs through the middle of the lateral surface of the pericardium and should be sharply mobilized off the pericardium to allow for tension free retraction and a wider access to the pericardial surface (Video 2). Alternatively the pericardium can be divided anterior and posterior to the phrenic nerve leaving it on an island of pericardium. This is done when a left sided pericardiectomy is to be performed. On the right the phrenic nerve is just anterior to the hilum of the lung and does not interfere with pericardial resection (Video 1).
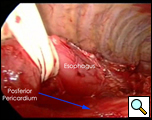
The pulmonary ligament is mobilized with cautery after grasping the lower lobe and retracting it superiorly (Video 4). This allows greater exposure of the pericardium and allows the lower lobe to be retracted out of the operative field. If the posterior pericardial space is to be accessed then the posterior mediastinal pleura is opened from the level of the inferior pulmonary vein to the main stem bronchus. On the right the esophagus will have to be mobilized to improve the exposure (Figure 5). Blunt dissection with a tonsil sponge stick allows the pericardium to be separated from the surrounding soft tissue.
 |
 |
 |
| Figure 5. Access to posterior pericardium. | Figure 6a. Long curved Allis clamp. | Figure 6b. Retraction of pericardium by Allis clamp. |
Often the pericardium is distended or thickened and it is easiest to grasp it with a curved long Allis clamp (Figure 6) introduced through the working incision at a point anterior to where the initial incision is to be made and retracting it anteriorly or laterally to tent the pericardium (Video 5). If the pericardium is too distended to allow this, aspiration of the effusion using a spinal needle introduced through the chest wall under thoracoscopic vision is performed. Alternatively, a needle for aspiration at the time of mediastinoscopy can be used.
A scissors is used to open the pericardium starting posteriorly and superiorly at the level of the superior pulmonary vein and then continuing inferiorly in a vertical line to the diaphragm (Video 6). This line of incision is anterior to the phrenic nerve. Bleeding from the cut pericardial edge is controlled with mono- or bipolar cautery. The underlying heart is protected with a peanut dissector to avoid causing ventricular fibrillation or tachycardia; alternatively, the pericardial edge is retracted away from the heart when the cautery is applied (Video 7). If an arrhythmia occurs then external cardioversion is performed.
If the pericardium is very thickened or vascular, an endoGIA (30 2.5mm) vascular stapler can be used to extend the incision after the initial pericardial opening is made (Video 8). Adhesions between the heart and the pericardium may be dissected sharply with scissors or bluntly using a peanut or Yankauer sucker, depending on the density or tenacity of the adhesion (Video 9). The incision in the pericardium is then carried medially towards the sternum. The same is done at the superior end of the incision. The substernal plane can be dissected with cautery across the midline or to the contralateral chest depending on the size of the window to be created or if a pericardiectomy is to be performed. The attached margin of the pericardium is resected either sharply, using cautery, or with a stapler. The free margin is grasped and pulled towards the surgeon, exposing the inferior cut edge of the pericardium, at which point the resection is started working superiorly until the pericardium to be removed is completely free (Video 10). The opening in the pericardium should be at a minimum approximately 4x4cm in size to ensure that the pericardial space will be adequately drained (Figure 7; Video 11).
 |
 |
| Figure 7a. Representative size of pericardial specimen. a: intraoperative view | Figure 7b. resected specimen |
When the posterior pericardial space is to be accessed, the incision on the pericardium can be made posterior to the pulmonary veins and a piece of pericardium is resected by the technique described. The posterior space is more easily accessed through the right chest as the esophagus can be mobilized to facilitate the exposure.
Once the window has been created, a Yankauer sucker is used to probe the pericardial space to ensure complete drainage of the effusion and to break down fibrous septa that may prevent complete drainage. A 28 Fr chest tube or a No.19 Blake drain is placed in the pericardiopleural space and brought out through the camera port incision (Video 12). Once the drainage is less than 200cc/24hrs it is removed.
Preference Card
• 30 degree thoracoscope
• Long curved Allis clamp
• Aspirating needle used for mediastinoscopy
• Thoracoscopic scissors
• EndoGIA with vascular staple load
• Peanut dissector and tonsil sponge
• Yankauer sucker
• External defibrillator pads
Tips & Pitfalls
- Place defibrillator pads on the patient while positioning.
- If the patient is unstable perform a subxiphoid window.
- Aspirate the effusion if the pericardium is distended and use the Allis clamp to grasp the pericardium
- Use cautery at low setting when resecting the pericardium and protect the heart with a peanut dissector or sucker. Keep the phrenic nerve in view.
- Resect an adequate area of pericardium.
- Ensure there are no undrained areas of the pericardial space by using a sucker to explore all areas.
Results
A thoracoscopic approach to pericardial window or resection allows for better exposure and visualization of the pericardium, resulting in a more generous resection without the morbidity of thoracotomy or sternotomy. The durability of the window has been shown to be longer than that of a subxiphoid approach, although this approach is the least morbid [4,5]. Other minimally invasive techniques employ a video-assisted subxiphoid or an uniportal thoracoscopic pericardial window approach [6].
Until recently, patients in tamponade were considered unsuitable for a thoracoscopic window. However, a recent series noted no difficulties when patients with tamponade had a window performed thoracoscopically [5]. It has also been shown to be applicable in stable trauma patients with hemopericardium [7] and for delayed post cardiotomy effusions.
A window can be performed from either side and the decision should be individualized.
Prevention of ventricular arrhythmias is important; however, this event is unreported in clinical series and the risk is probably minimal.
The resection can be with scissors, cautery, a stapling device, or a harmonic scalpel, with no one technique demonstrably better than another. It is best to have a combination of techniques available to resect the pericardium adequately.
Chest tubes are removed in 2-3 days once the drainage is less than 200cc/24hrs and the patient discharged in the same time frame.
Video 1
Echo 1
Video 2
Video 3
Video 4
Video 5
Video 6
Video 7
Video 8
Video 9
Video 10
Video 11
Video 12
References
- Krasna M, Mack M. Atlas of Thoracoscopic Surgery. 2nd ed. c1994. Pericardial Window; p. 27-37.
- Watanabe S, Kariatsumari K, Sakasegawa K, Imagama I, Yotsumoto G, Sakata R. Primary chylopericardium treated with video-assisted thoracoscopic surgery. Thorac Cardiovasc Surg 2002;50:360-1.
- Katara AN, Samra SS, Bhandarkar DS. Thoracoscopic window for a post-coronary artery bypass grafting pericardial effusion. Indian Heart J 2003;55:180-1.
- Liberman M, Labos C, Sampalis JS, Sheiner NM, Mulder DS. Ten-year surgical experience with nontraumatic pericardial effusions: a comparison between the subxyphoid and transthoracic approaches to pericardial window. Arch Surg 2005;140:191-5.
- O'Brien PK, Kucharczuk JC, Marshall MB, Friedberg JS, Chen Z, Kaiser LR, Shrager JB. Comparative study of subxiphoid versus video-thoracoscopic pericardial "window". Ann Thorac Surg 2005;80:2013-9.
- Rocco G, La Rocca A, La Manna C, Scognamiglio F, D'Aiuto M, Jutley R, Martucci N. Uniportal video-assisted thoracoscopic surgery pericardial window. J Thorac Cardiovasc Surg 2006;131:921-2.
- Navsaria PH, Nicol AJ. Video-assisted thoracoscopic pericardial window for penetrating cardiac trauma. S Afr J Surg 2006;44:18-20.



