ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Three-Step Myectomy, Mitral Plication, and Chordae Cutting for Hypertrophic Cardiomyopathy Through a Transaortic Approach
Vrancic JM, Cervetti MR, Chiappe MA, Benavidez J, Clusa NM, Navia D. Three-Step Myectomy, Mitral Plication, and Chordae Cutting for Hypertrophic Cardiomyopathy Through a Transaortic Approach. September 2018. doi:10.25373/ctsnet.7073015.
The patient was a 61-year-old man with hypertrophic obstructive cardiomyopathy with severe heart failure symptoms (New York Heart Association functional class III). His cardiovascular history included dyslipidemia, smoking, and the death of his father by sudden death. Transthoracic echocardiography showed mild septal hypertrophy (17 mm) confined mainly to anterior, lower-basal, and medium portions of the septum, systolic anterior motion (SAM) of the anterior leaflet of the mitral valve (MV) with mitral septal contact, and moderate left atrial dilation (46 ml/m2). Doppler echocardiography revealed an outflow tract gradient of 80 mm Hg at rest, and the gradient increased to 122 mm Hg upon Valsalva maneuver.
Systematically, in the operating room and prior to incision, the intraoperative transesophageal echocardiogram (TEE) was reviewed. A standard median sternotomy was preferred to provide adequate access to both the aorta and the left ventricle. The patient was placed on cardiopulmonary bypass using moderate hypothermia (32 degrees Celsius). The aorta was cross-clamped, and anterograde and retrograde cold crystalloid cardioplegia was delivered. After transverse aortotomy and retraction of the aortic valve leaflets, the extent of septal hypertrophy and the mitral valve were evaluated.
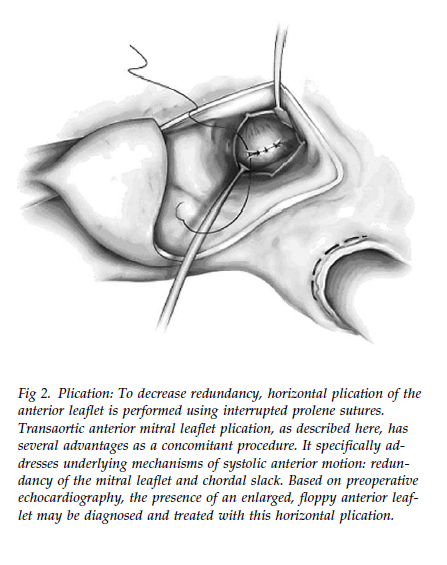
The authors proceeded to perform the extended myectomy of the basal septum but without exceeding a thickness of 5 mm, given the 17 mm thickness observed on imaging. Briefly, two parallel incisions were made 8 - 10 mm below the nadir of the right coronary valve, extending to the base of the papillary muscles in the form of a trapezoid. The resection was completed apically, and continued to the left to the anterior leaflet of the MV and to the right to the medial postoperative commissure. Two second-order chordae of the anterior valve were resected. Finally, the authors plied the anterior mitral valve using three separate stitches with proline 5-0 sutures. To determine the extent of plication, they integrated the preoperative echo, the degree of SAM, the size of the mitral valve, and the slack and redundancy of the anterior leaflet as assessed with the nerve hook. In general, this results in a plication of 2 - 5 mm, depending on the amount of redundancy and the size of the anterior leaflet.
After final inspection, and irrigation and suctioning to remove any possible residual loose pieces of muscle, the aortotomy was closed with a running 5-0 proline suture as the patient was rewarmed and the heart allowed to fill passively with blood. Standard de-airing was carried out as the cross-clamp was removed. As soon as contractility was restored, the result could be assessed by either partial bypass or temporarily suspending it altogether. Adequacy of the resection and mitral insufficiency was examined.
Intraoperative TEE showed that the MV coaptation point had moved away from the left ventricular outflow tract to a more posterior and normal position within the left ventricular cavity, and that the MV SAM and MV regurgitation were absent. The sternotomy was closed in a standard fashion. The patient had a normal echocardiogram with adequate gradients at a follow-up visit one month postoperatively.
Video References
- Balaram SK, Sherrid MV, Derose JJ Jr, Hillel Z, Winson G, Swistel DG. Beyond extended myectomy for hypertrophic cardiomyopathy: the resection-plication-release (RPR) repair. Ann Thorac Surg. 2005;80(1):217-223.
- Ralph-Edwards A, Vanderlaan RD, Bajona P. Transaortic septal myectomy: techniques and pitfalls. Ann Cardiothorac Surg. 2017;6(4):410-415.




Comments