ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
VATS Mediastinal Nodal Dissection
Patient Selection
The majority of patients selected for VATS mediastinal nodal dissection are patients undergoing VATS lobectomy procedures for malignancy. Nodal drainage patterns have been described and are depicted in Figures 1 & 2 [1]. All ipsilateral nodal regions are accessible by the VATS approach [2] and we routinely perform two-station mediastinal lymph node dissections or sampling during all VATS lobectomies for malignancy. Currently we are performing VATS lobectomy only for suspected stage IA tumors. VATS mediastinal nodal dissection can be performed in any situation where mediastinal nodal evaluation (either dissection or sampling) is required [3, 4]. When resecting primary lung tumors, at minimum a lymph node sampling from appropriate stations should be performed.
 |
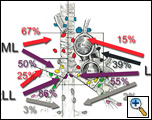 |
| Figure 1: Distribution of spread to the mediastinal lymph nodes for the upper lobes. | Figure 2: Distribution of spread to the mediastinal lymph nodes for the middle and lower lobes. |
Operative Steps
The patient is positioned in the lateral decubitus position with the table maximally flexed with additional slight reverse Trendelenburg to make the patient’s torso parallel to the floor. Most commonly the lymph node dissection is performed after the lobectomy specimen is removed
Right level 2/4 Nodal Dissection
The first step is to divide the azygous vein. To accomplish this, the lung is retracted inferiorly and a large blunt right-angled clamp is used to dissect behind the azygous vein. Once the vein is adequately mobilized an endovascular stapler is placed through the posterior port to transect the vein. A wide spreading curved ring forceps is placed through the posterior port. The trachea and superior vena cava are retracted away from each other allowing easy access into the paratracheal nodal area. The mediastinal pleura overlying the level 2 or 4 area is incised using electrocautery. The nodal tissue is dissected off the lateral wall of the superior vena cava up to the level of the right subclavian artery. The most inferior portion of the nodal packet is grasped with a ring forceps at the tracheobronchial angle (care must be taken not to injure the truncus branch of the pulmonary artery). The packet is lifted superiorly off the underlying pericardium while electrocautery and endoclips are used for control of blood vessels and lymphatics. The entire packet is placed in a specimen retrieval bag and removed via the utility incision.
Level 7 nodal dissection (right)
The lung is retracted medially and the posterior mediastinal pleura is divided using electrocautery. Identification of the posterior aspect of the inferior pulmonary vein marks the starting point of the dissection. At this point the bronchus intermedius/right mainstem bronchus should be visible. An empty ringed forceps is used to grasp the inferior portion of the level 7 nodal packet and retract it superiorly. Sharp dissection and electrocautery are used to dissect the nodal packet off the posterior pericardium and laterally until the left mainstem bronchus is visualized. Care must be taken not to injure the vagus nerve and the esophagus. Once the inferior portion of the nodal chain is elevated, the nodal packet is grasped in its entirety and dissection is continued superiorly using electrocautery and clips until the carina is clearly visualized. The nodal packet is then placed in a bag and removed via the utility incision
Level 7 nodal dissection (left)
Similar to the right side, the left lung is retracted medially and the posterior mediastinal pleura is divided using electrocautery. Again, the key is to first identify the posterior portion of the left lower lobe vein. The lung must be retracted with a bit more force than on the right because the carina rests behind the aorta and esophagus. After the left main stem bronchus is identified, a curved ring forceps is placed between the left mainstem bronchus and esophagus and opened widely. The same forceps is then placed through the utility incision to grasp the nodal packet. It is retracted superiorly towards the carina. It is difficult to visualize the right mainstem bronchus with the left lower lobe in place, especially with the left lower lobe vein intact. This left sided subcarinal nodal dissection is significantly easier during a left lower lobectomy because the dissection is facilitated by division of the left lower lobe vein. The main technical point is that adequate retraction on the lung and proper placement of the ring clamp is essential to the successful completion of the subcarinal nodal dissection from the left side.
Level 5 and 6 Nodal Dissection
The pleura overlying the aortopulmonary window is divided transversely; care must be taken to avoid injuring the vagus (left recurrent nerve) and the phrenic nerve. The superior edge of the pleura is retracted superiorly exposing the underlying great vessels and lymph nodes. A curved ring clamp grasps the lymph nodes as well as some surrounding fat, and sharp dissection and electrocautery are used to dissect the nodal tissues off the underlying pulmonary artery for level 5 and the aorta for level 6. The specimen is placed in a retrieval bag and removed.
Level 8 and 9 Nodal Dissection
During the mobilization of the pulmonary ligament an empty ring clamp is used to grasp the level 9 or level 8 lymph nodes. These are retracted away from the mediastinum and easily excised using electrocautery. Caution should be used to prevent injury to the esophagus and accompanying vagus nerve.
Preference Card
• 30 degree thoracoscope
• Long curved ring clamp
• Large right angled clamp
• Long Metzenbaum scissors
• Packing forceps
• Weitlaner retractor
• Specimen retrieval bag
• Sponge stick with open thoracotomy tray immediately available
Tips & Pitfalls
• Always have a sponge on a stick, an open thoracotomy tray, and sutures ready for emergency control of hemorrhage
• During right sided subcarinal lymph node dissection use caution to avoid injury to the esophagus
• For level 5 and 6 nodal dissection one must always beware of the left recurrent laryngeal nerve.
• Always identify the phrenic nerve prior to either right or left sided nodal dissections.
Results
We have performed over 130 VATS lobectomies, and our technique of lymph node dissection has evolved accordingly. Although we have not done so, other authors have demonstrated that nodal dissection via the VATS approach is comparable to nodal dissection through a thoracotomy [2]. We have not seen any specific complications directly related to our method of lymph node dissection and the addition of a 2-field VATS lymph node dissection adds an additional 30-40 minutes to the procedure.
The issue of whether to perform a lymph node dissection or sampling is unresolved although recent reports suggest that a thorough lymph node dissection may improve disease–free survival when compared to only sampling [5]. For this reason, we continue to perform lymph node dissections in all cases where a cancer is identified.
Acknowledgment: The author would like to thank Robert McKenna, MD for allowing him to observe his operative technique.
References
- Asamura H, Nakayama H, Kondo H, Tsuchiya R, Naruke T. Lobe-specific extent of systematic lymph node dissection for non-small cell lung carcinomas according to a retrospective study of metastasis and prognosis. J Thorac Cardiovasc Surg 1999;117:1102-11.
- Sagawa M, Sato M, Sakurada A, Matsumura Y, Endo C, Handa M, Kondo T. A thoracic surgery: can it be perfect? Ann Thorac Surg 2002;73:900-4.
- McKenna RJ Jr, Wolf RK, Brenner M, Fischel RJ, Wurnig P. Is lobectomy by video-assisted thoracic surgery an adequate cancer operation? Ann Thorac Surg 1998;66:1903-8.
- Walker WS, Codispoti M, Soon SY, Stamenkovic S, Carnochan F, Pugh G. Long-term outcomes following VATS lobectomy for non-small cell bronchogenic carcinoma. Eur J Cardiothorac Surg 2003;23:397-402.
- Lardinois D, Suter H, Hakki H, Rousson V, Betticher D, Ris HB. Morbidity, survival, and site of recurrence after mediastinal lymph-node dissection versus systematic sampling after complete resection for non-small cell lung cancer. Ann Thorac Surg 2005;80:268-74.




Comments