ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Left Ventricular Assist Device Exchange: Replacement of a HeartMate XVE with a HeartMate II Device
Index
Index
» Operative Steps
» Postoperative Care
» References
Related Items
Surgical Implantation of the Heartmate II Left Ventricular Assist Device [Video]
Implantation of TCI Heartmate Left Ventricular Assist System: Keys to Success [Technique]
World's first internal transplant of a miniature LVAD performed at Texas Heart Institute.(Brief Article): An article from: Transplant News [CTSNet Amazon Bookstore]
“On Trial 2009” [Research]
Off-Pump Insertion of the Jarvik 2000 Left Ventricular Assist Device [Technique]
Small Assist Device Used in Emergency Case as Twin, Heart Booster Pumps for First Time in U.S. [JANS]
Left Ventricular Assist Device: Webster's Timeline History, 1972 - 2007 [CTSNet Amazon Bookstore]
This article describes how a HeartMate XVE left ventricular assist device may be exchanged for a HeartMate II axial-flow pump with low morbidity and mortality and without a full sternotomy.

In the United States, at least 5 million persons have heart failure at any given time, and more than 550,000 new cases of heart failure are diagnosed each year. Almost 20% of heart failure patients require intravenous inotropic therapy, left ventricular assist device (LVAD) therapy, and/or cardiac transplantation (1). Because the latter option is limited by the scarcity of donor hearts (2) and because LVAD therapy has been shown to result in superior survival in heart failure patients ineligible for transplantation (3), implantable LVADs are being used with increasing frequency and for longer periods. These devices include the HeartMate XVE LVAD (HM-XVE) (Thoratec Corporation, Pleasanton, California) (4), a pulsatile pump that has been approved by the United States Food and Drug Administration for destination therapy. In contrast, newer, axial-flow LVADs—such as the HeartMate II (HM-II) (Thoratec)—are smaller, more reliable, and more durable than current pulsatile pumps and, therefore, suitable for a broader patient population.
Experience has shown that the HM-XVE LVAD offers durable and reliable mechanical support in the first year but has a high risk of life-threatening failure after 18 to 24 months (5). Reoperative surgery in these patients can be challenging, especially when pump failure necessitates urgent device exchange. In our early experience with HM-XVE exchange, we performed a redo sternotomy to optimally expose the outflow graft. As we gained experience with the exchange procedure, however, we found that we could expose enough of the pump and graft by performing a left subcostal incision and extending it slightly past the midline, thereby avoiding a full sternotomy (6). With this approach, exchanging a HM-XVE for the HM-II axial-flow pump can be accomplished with low morbidity and mortality.
Operative Steps
- After endotracheal anesthesia has been induced and a transesophageal echocardiography probe inserted, the patient is placed in the supine position, with the groin easily accessible for cardiopulmonary bypass cannulation.
- The common femoral artery and common femoral vein are exposed surgically and are cannulated by means of the Seldinger technique, using a 21F cannula for arterial cannulation and a 30-32F cannula for venous cannulation (Fig. 1).
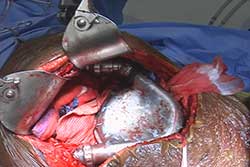
- A left subcostal incision is performed and is extended 2 cm to the patient’s right side as a limited chevron incision (Fig. 2). The incision is continued downward directly to the HM-XVE’s hardware pocket. By confining dissection to the pump pocket, one can avoid entering abdomen. A Thompson retractor provides excellent exposure (Fig. 3).
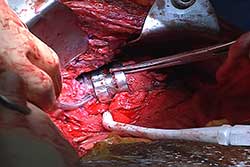
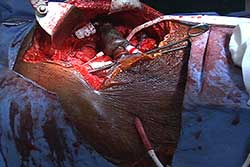
- Dissection is performed to expose the HM-XVE inlet and outlet cannulas, as well as the outflow graft and the LVAD itself (Fig. 4). If the outflow graft cannot be adequately exposed in this manner, a right anterior minithoracotomy is performed to expose the outflow graft in the chest. Once an adequate length of outflow graft is available for clamping and creation of a graft-to-graft anastomosis, attention is turned to the inlet cannula.
- The inlet cannula is dissected to expose the base of the sewing ring and the Silastic inlet, in its entirety. Limited dissection of the diaphragm surrounding the inlet is done around the apex to give the surgeon enough mobility to fully expose the inflow cannula, which is secured with electrician’s tape (Fig. 5).
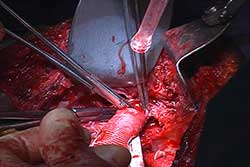
- Full heparinization is instituted, and the patient is placed in the Trendelenburg position. Cardiopulmonary bypass is started, and the HM-XVE LVAD is turned off. By dividing the driveline, one can attain mobility of the whole LVAD (Figs. 6 and 7), which can further assist in the sometimes difficult task of exposing the sewing ring base. The outflow graft is clamped and divided, leaving enough of a rim to anastomose it to the HM-II’s outflow graft. The electrician’s tapes are cut and removed gently without damaging the inlet cannula (sewing-ring Silastic tube). The pump’s inlet cannula is then gently removed from the Silastic inlet cuff.
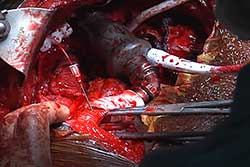
- During this period, the presence of air in the ventricle and ascending aorta is monitored continuously with transesophageal echocardiography. The HM-II inlet cannula is inserted into the inflow cannula and secured with electrician’s tape (Fig. 8). The HM-II outflow graft is cut to an appropriate length, leaving a beveled edge. A graft-to-graft anastomosis to the HM-XVE outflow graft is then created with continuous, running 5-0 polypropylene sutures (Fig. 9). Both the LVAD and the left ventricle are de-aired (Fig. 10).
- The HM-II’s driveline is tunneled toward the right subcostal area and brought out just above the exit site of the HM-XVE driveline (Fig. 11). A single 36F chest tube is inserted. Meticulous control of bleeding is essential. Because all patients undergoing device exchange will develop a coagulopathy, only the skin is closed. The next day, the patient is returned to the operating room for washout of the abdominal incision site, closure of the abdomen, and removal of the HM-XVE driveline.
Postoperative Care
Postoperatively, appropriate antibiotic prophylaxis is carried out with broad coverage, including an antifungal agent. The chest tube can usually be removed the day after surgery. Anticoagulant therapy is then started according to our protocol (7). Nasogastric-tube suction should be continued until the patient’s bowel activity is resumed, after which the nasogastric tube is removed and oral feeding begun, as tolerated.
Surgical Tips and Pitfalls
- By removing the xiphoid, the surgeon can better mobilize and expose the outflow graft of the HM-XVE.
- If the HM-XVE device was placed intraabdominally, it is safest to enter the abdomen at the level of the liver to prevent injury of nearby organs.
- If an HM-XVE LVAD pocket is present, cultures should be obtained for intraoperative gram-stain analysis. If there is any possibility of infection, the replacement LVAD should be inserted intraabdominally.
Comment
We have found that the pulsatile HM-XVE LVAD can be exchanged for the newer, axial-flow HM-II pump with low morbidity and mortality. According to Lietz and coworkers (8), the likelihood of device exchange or fatal device failure is 17.9% and 72.9% at 1 and 2 years, respectively. Because our subcostal approach entails shorter operative and recovery times and fewer transfusion requirements (9), it simplifies the exchange procedure while precluding the need for a median sternotomy.
References
- Hunt SA, Baker DW, Chin MH, et al. ACC/AHA Guidelines for the Evaluation and Management of Chronic Heart Failure in the Adult: Executive Summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1995 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the International Society for Heart and Lung Transplantation; endorsed by the Heart Failure Society of America. Circulation 2001;104:2996-3007.
- Hosenpud D, Bennett LE, Deck BM, et al. The registry of the International Society for Heart and Lung Transplantation; seventeenth official report—2000. J Heart Lung Transplant 2000;12:909-31.
- Rose EA, Gelijns AC, Moskowitz AJ, et al, for the Randomized Evaluation of Mechanical Assistance for the Treatment of Congestive Heart Failure (REMATCH) Study Group. Long-term mechanical left ventricular assistance for end-stage heart failure. N Engl J Med 2001;345:1435-43.
- Dowling RD, Park SJ, Pagani FD, et al. HeartMate VE LVAS design enhancements and its impact on device reliability. Eur J Cardiothorac Surg 2004;25:958-63.
- Martin J, Friesewinkel O, Benk C, et al. Improved durability of the HeartMate XVE left ventricular assist device provides safe mechanical support up to 1 year but is associated with high risk of device failure in the second year. J Heart Lung Transplant 2006;25:384-90.
- Frazier OH, Forrester MD, Gemmato C, Gregoric ID. Urgent pump exchange for stroke resulting from a distorted HeartMate XVE inflow conduit. J Heart Lung Transplant 2007;26:646-8.
- Offer Amir, MD, Arthur W. Bracey, MD, Frank W. Smart. A successful anticoagulation protocol for the first HeartMate II implantation in the United States. Tex Heart Inst J 2005;32:399–401.
- Lietz K, Long JW, Kfoury AG. Outcomes of left ventricular assist device implantation as destination therapy in the post-REMATCH era: implications for patient selection. Circulation 2007;116:497-505.
- Gregoric ID, Bruckner BA, Jacob L. Clinical experience with sternotomy versus subcostal approach for exchange of the HeartMate XVE to the HeartMate II ventricular assist device. Ann Thorac Surg 2008;85:1646-9.