ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Current Status of Tricuspid Interventions
Taramasso M, Zancanaro E. Current Status of Tricuspid Interventions. April 2023. doi:10.25373/ctsnet.22438780.v1
This article is part of CTSNet’s Guest Editor Series, 21 Years After First TAVI: Will Pace of Innovations Continue for All Heart Valves? Guest editor Gry Dahle has curated a robust collection of content that shares the knowledge, techniques, and insights of several distinguished experts from around the world.
Current Status of Tricuspid Valve Treatment
Tricuspid valve (TV) treatment, at its current status, represents a real dilemma since different options are available but long-term results still to be seen and lots of new strategies are still to come.
The current gold standard treatment is represented by TV surgery, particularly in two different cases:
1) Concomitant tricuspid surgery at the time of left-side valve surgery, which goes beyond the present paper’s scope.
2) Isolated tricuspid valve surgery: late tricuspid regurgitation (TR), atrial TR due to annular dilatation, organic or iatrogenic (lead induced) TR, and endocarditis induced TR were distinguished. The first two mentioned represented the most frequent cases (90 percent in Europe and the US) and will be the focus of this analysis.
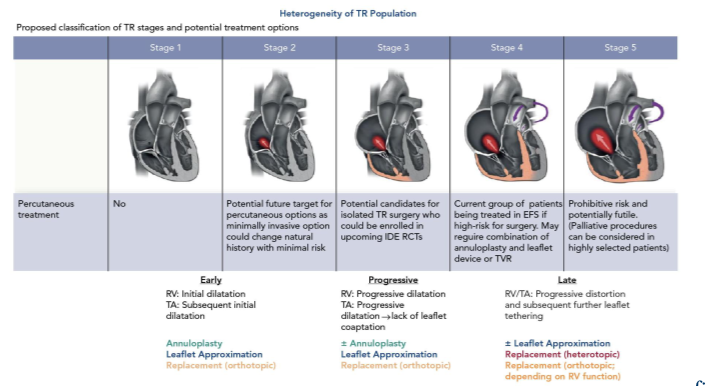
TR is a progressive disease, and if the treatment is delayed the annulus, which is the more prominent cause of TR, will progressively dilate and severely damage the valve, leading to a more complicated clinical condition; Table 1 shows schematically TR progression stages. The take-home message is that TR should be addressed as early as possible.
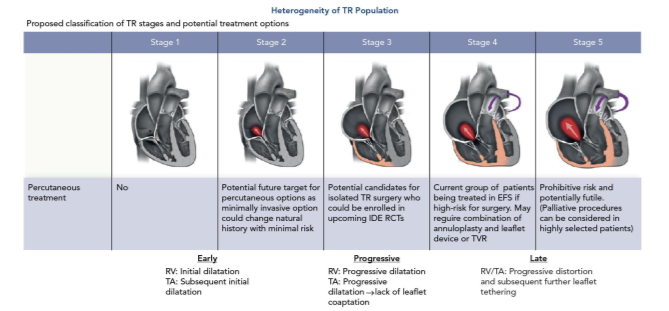
Figure 1 puts into relation the five different TR progression stages with the surgical treatment options that are currently available. Interestingly enough, if the annulus is too dilated, it’s recommended to replace the valve with a prosthesis in order to avoid TR recurrence (which is around 20 percent for TV repair at that stage).
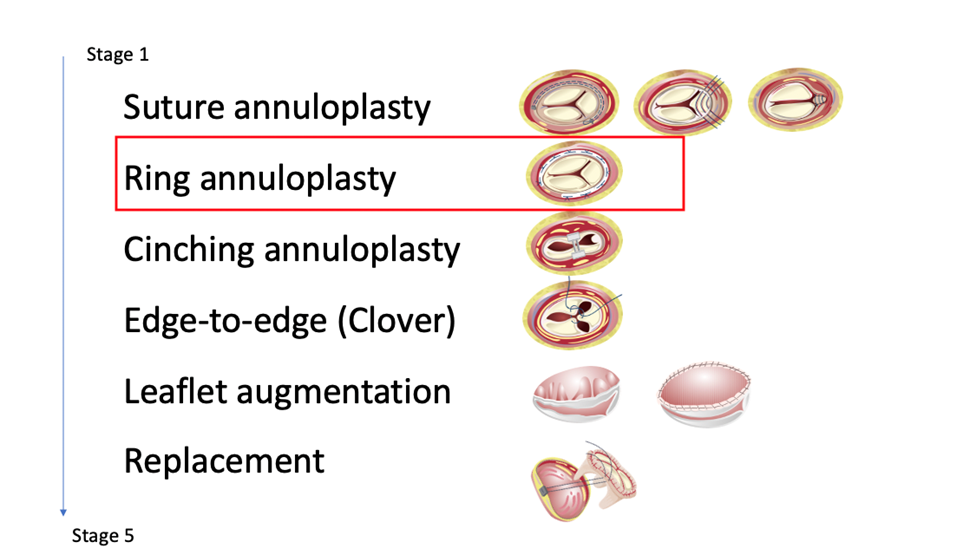
Concerning the surgical technique, there has been an important improvement in ring types for TV annuloplasty (incomplete three-dimensional rings, etc.) (1).
Nevertheless, Zack et. al. demonstrated still an elevated range of in-hospital mortality (9 percent) despite the technological improvement (2). The reason for this not well-established result resides in the fact that TV pathology is addressed too late and the patient’s presentation is too critical with respect to those who arrive with less advanced disease (3).
The European Society of Cardiology (ESC) guidelines suggest a more precocious treatment of TV pathology considering the right ventricular function and preventing its severe dilatation (4). The guidelines look not only at TV surgical treatment but also at the emerging field of transcatheter repair.
Transcatheter Tricuspid Valve Repair
The present study will focus on the three principal devices for TV repair with CE approval: TriClip (Abbott), PASCAL (Edwards Lifesciences), and Cardioband (Edwards Lifesciences).
TriClip
The TriClip System is a transfemoral transcatheter edge-to-edge repair (TEER) system that facilitates the reconstruction of an insufficient tricuspid valve through tissue approximation. The repair creates a tissue bridge reducing the vale area and regurgitation jet.
At the moment, the TriClip is available in four different configurations: G4 NT/NTW and G4 XT/XTW (depending on the clip sizes) allowing an independent grasping of the TV leaflets.
Concerning the results, the Triluminate trial showed the two-year outcome after TV TEER (5).
Even though the Triluminate patients were deeply selected and thus do not reflect completely the real practice results, the trial showed an important TR reduction of >1+ or more in 85.4 percent of cases at thirty days and maintained at two years. This reflects good results in the long term not only in the TR reduction but also in the functional status and in hospitalization rate (5).
The TriClip bRight study showed that 90 percent of patients had TR reduction by at least one grade and 60 percent with a reduced TR to moderate or less, showing good safety of the device itself (6).
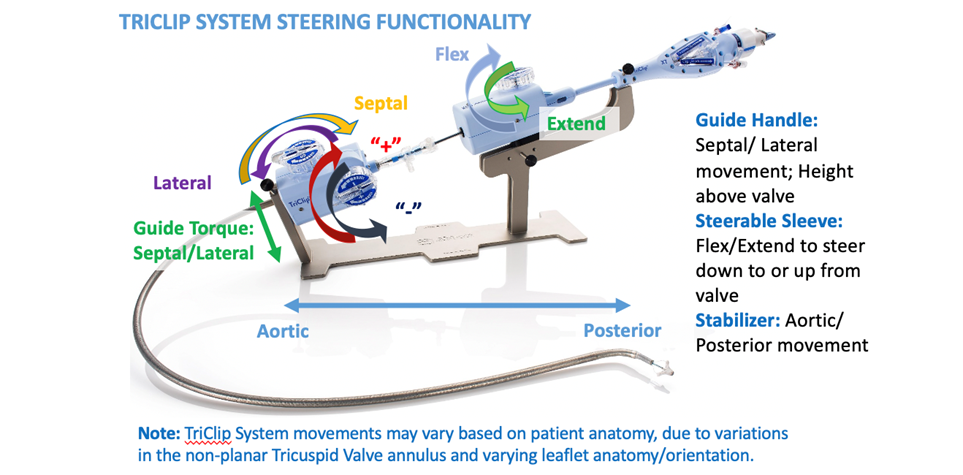
Concerning the structural part of TriClip, Figure 2 illustrates the principal components. The device is very similar to the MitraClip (Abbott) device with some modifications, as the steering part has been moved more on the guiding catheter and the adjunctive nobe (S/L) that helps the operator to increase the leaflets grasping capability due to a better coaxial projection.
The most important key points concerning correct TriClip positioning are:
1) The trajectory has to be perpendicular to the TV plane. This can be done by using the S/L and F/E nobe.
2) The clip should be placed perpendicular to the coaptation line of the target lesion. This is particularly important to prevent any kind of leaflet distortion.
PASCAL
The PASCAL (Edwards Lifesciences) is a transfemoral TEER device that acts similarly to TriClip G4 with the independent grasping of the leaflets. This same device can be used for TR and for mitral valve repair.
The first commercial multicenter study focused on PASCAL results for TR, showed a TR reduction < 2+ in 77 percent of patients and TR reduction > 1+ in 92 percent of cases (7). Also, the functional status (NYHA class and 6mwt) showed a significant improvement.
An interesting example of PASCAL implantation is shown in the video associated.
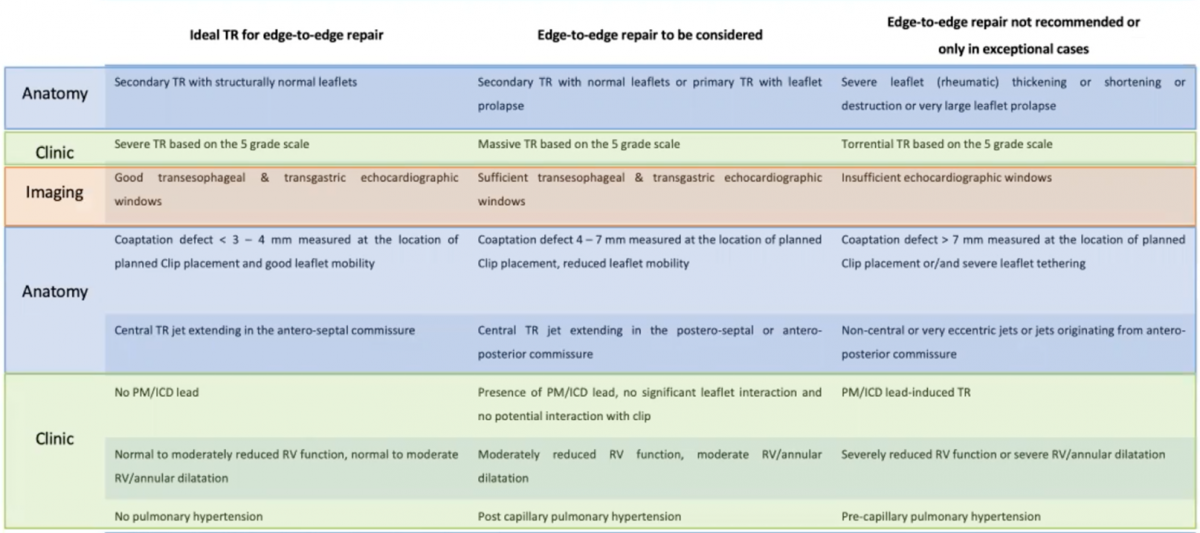
What is really mandatory in TEER procedure (TriClip and PASCAL) is the patient selection. Table 2 shows what patient selection should look like. The imaging section is particularly important and can be a useful guide in TEER visualization and positioning.
Cardioband
Cardioband (Edwards Lifesciences) is a transfemoral annuloplasty device. The rationale of this device is to implant a band from the anteroseptal commissure in a clockwise fashion. It is particularly indicated in central TR with the aim of recreating a normal coaptation.
Concerning the results, Cardioband showed 100 percent procedural success and 77 percent did not have major complications at thirty days (8). Interestingly enough, TR reduction and functional status at follow-up showed a similar result compared to TEER devices (8).
When TV Cannot Be Repaired
There are cases in which the aforementioned devices cannot be used for TV repair. The principal reasons are pacemakers that lead to induced TR and annular dilatation that is too severe.
In these cases, a different approach must be chosen: heterotopic tricuspid valve implantation (Tricento and Tricvalve). In both cases, the TV is left in place.
In Tricvalve the prosthesis is implanted into the superior and inferior vena cava, and in Tricento it is in the right atrium. They represent a symptomatic treatment since they reduce pressure in the venous system and at the liver level.
Concerning preprocedural planning, cardiac computed tomography (CT) is the gold standard.
TV Replacement
A novel platform in the case of TV replacement is represented by the Evoque valve (Edwards Lifesciences). It is a transfemoral implantable valve.
The key point of this device is the abolishment of TR with good safety results (9).
Conclusion
The final important concept is to shape the correct TV treatment according to the TR stage, which can be seen in Table 3. As said before, the more critical the stage becomes, the more TV replacement becomes the real option.
The final question is: Does transcatheter tricuspid valve intervention improve survival (10)?
Promising results are seen, but in the end, ongoing randomized trials will give more answers to lots of questions that are still making TV treatment a real dilemma.
References
- Davide Carino, Edoardo Zancanaro, Elisabetta Lapenna, Stefania Ruggeri, Paolo Denti, Giuseppe Iaci, Nicola Buzzatti, Maria Chiara Calabrese, Simona Nascimbene, Alessandra Sala, Alessandro Castiglioni, Ottavio Alfieri, Michele De Bonis, Long-term results of tricuspid annuloplasty with 3-dimensional-shaped rings: effective and durable!, European Journal of Cardio-Thoracic Surgery, Volume 60, Issue 1, July 2021, Pages 115–121, https://doi.org/10.1093/ejcts/ezab111.
- Zack C, Fender E, Chandrashekar P, et al. National Trends and Outcomes in Isolated Tricuspid Valve Surgery. J Am Coll Cardiol. 2017 Dec, 70 (24) 2953–2960. https://doi.org/10.1016/j.jacc.2017.10.039.
- Kim JB, Jung S, Choo SJ, et al Surgical outcomes of severe tricuspid regurgitation: predictors of adverse clinical outcomes Heart 2013;99:181-187.
- Vahanian, A. et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease: Developed by the Task Force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Rev. Esp. Cardiol. Engl. Ed. 75, 524 (2022).
- Lurz P, Stephan von Bardeleben R, Weber M, et al. Transcatheter Edge-to-Edge Repair for Treatment of Tricuspid Regurgitation. J Am Coll Cardiol. 2021 Jan, 77 (3) 229–239. https://doi.org/10.1016/j.jacc.2020.11.038.
- E Donal, R Shueler, B Goebel, H Lapp, H Moellmann, G Nickenig, R Bekeredjian, R Estevez, I Atmowihardjo, A Schmeisser, M Kowalski, P Trusty, P Lurz, Real-world outcomes for tricuspid edge-to-edge repair: initial echocardiographic results from the TriClip bRIGHT study, European Heart Journal - Cardiovascular Imaging, Volume 23, Issue Supplement_1, February 2022, jeab289.203, https://doi.org/10.1093/ehjci/jeab289.203.
- Wild MG, Löw K, Rosch S, Gerçek M, Higuchi S, Massberg S, Näbauer M, Rudolph V, Markovic S, Boekstegers P, Rassaf T, Luedike P, Geisler T, Braun D, Stolz L, Praz F, Lurz P, Hausleiter J; PASTE Investigators. Multicenter Experience With the Transcatheter Leaflet Repair System for Symptomatic Tricuspid Regurgitation. JACC Cardiovasc Interv. 2022 Jul 11;15(13):1352-1363. doi: 10.1016/j.jcin.2022.05.041. PMID: 35798479.
- Nickenig G, Weber M, Schüler R, Hausleiter J, Nabauer M, von Bardeleben RS, Sotiriou E, Schäfer U, Deuschl F, Alessandrini H, Kreidel F, Juliard JM, Brochet E, Latib A, Montorfano M, Agricola E, Baldus S, Friedrichs KP, Deo SH, Gilmore SY, Feldman T, Hahn RT, Maisano F. Tricuspid valve repair with the Cardioband system: two-year outcomes of the multicentre, prospective TRI-REPAIR study. EuroIntervention. 2021 Feb 5;16(15):e1264-e1271. doi: 10.4244/EIJ-D-20-01107. PMID: 33046437.
- Webb JG, Chuang AM, Meier D, von Bardeleben RS, Kodali SK, Smith RL, Hausleiter J, Ong G, Boone R, Ruf T, George I, Szerlip M, Näbauer M, Ali FM, Moss R, Kreidel F, Bapat V, Schnitzler K, Ye J, Wild M, Akodad M, Deva DP, Chatfield AG, Mack MJ, Grayburn PA, Peterson MD, Makkar R, Leon MB, Hahn RT, Fam NP. Transcatheter Tricuspid Valve Replacement With the EVOQUE System: 1-Year Outcomes of a Multicenter, First-in-Human Experience. JACC Cardiovasc Interv. 2022 Mar 14;15(5):481-491. doi: 10.1016/j.jcin.2022.01.280. PMID: 35272772.
- Taramasso M, Gavazzoni M, Pozzoli A, Dreyfus GD, Bolling SF, George I, Kapos I, Tanner FC, Zuber M, Maisano F, Hahn RT. Tricuspid Regurgitation: Predicting the Need for Intervention, Procedural Success, and Recurrence of Disease. JACC Cardiovasc Imaging. 2019 Apr;12(4):605-621. doi: 10.1016/j.jcmg.2018.11.034. PMID: 30947904.
Disclaimer
The information and views presented on CTSNet.org represent the views of the authors and contributors of the material and not of CTSNet. Please review our full disclaimer page here.



