Bronchoscopic alternatives to lung volume reduction surgery (LVRS) have been recently proposed; the airway bypass [1-3] and bronchoscopic lung volume reduction (BLVR) are certainly one step beyond current LVRS practice. In particular, BLVR with one–way valves has been attempted in the experimental laboratory [4] and in selected clinical settings [5-8]. The one–way valve allows air to be vented from the isolated lung segment during normal expiration and prevents air from refilling the lung during expiration. It has been postulated that the placement of these valves in the segmental bronchi could functionally isolate the airway that supplies the most hyperinflated parts of the emphysematous lungs, favoring deflation and even atelectasis, and thus mimicking LVRS in its contribution to alleviate symptoms.
 |
| Figure 1: First generation of endobronchial one–way valves. |
The Emphasys (Emphasys; Redwood City, CA; USA) endobronchial valve (EBV) is an endobronchial prosthesis designed to both control and redirect airflow. It is a one–way, polymer, duckbill valve that is mounted inside a stainless steel cylinder which is attached to a nickel–titanium (nitinol) self-expanding retainer (Figure 1). It prevents air from entering the target lung but allows air and mucous to exit. The EBV is provided in three sizes, each intended for a different range of target bronchial lumen diameters: 4.0/5.5 mm (inner/outer diameter), 5.0/7.0 mm, and 6.5/8.5 mm; each valve is 10 mm long.
These valves are usually placed in a general operating room setting, with the patient intubated under intravenous anaesthesia (Propofol infusion) and spontaneous assisted ventilation. After the patient is intubated, the flexible
 |
| Figure 2: Delivery catheter for the first generation of endobronchial one–way valves. |
bronchoscope is advanced into the endotracheal tube and the target bronchi are chosen. They correspond to the most hyperinflated part of the lung affected by heterogeneous emphysema as seen on computed tomography. The valves are usually placed in the segmental bronchi, but subsegmental orifices can also be stented to obtain complete lobar occlusion. A guidewire is inserted through the operating channel of the bronchoscope and left in place while the bronchoscope is withdrawn; a flexible delivery catheter (Figure 2) is guided to the target bronchus by the guidewire. Local anesthesia is generously administered before inserting the valves to prevent coughing. The fiberoptic bronchoscope is reinserted after the advancement of the delivery catheter; the tip of the delivery catheter containing the valve is pushed with a gentle rotation in the selected bronchial orifice, and the valve is delivered. Fiberoptic bronchoscopy performed after removal of the delivery catheter confirms the correct placement of the valve. Gentle suction through the bronchoscope ensures the correct opening of the valve to allow deflation of the lung and clearance of secretions (Video 1). No fluoroscopy is required. The valves can be removed easily if placement is not satisfactory using a rat–toothed grasper through the working channel of the bronchoscope.
The first generation of EBV have been extensively employed in several prospective, nonrandomized, single center longitudinal pilot studies to evaluate safety and short term efficacy with promising results in a selected group of patients with heterogeneous end stage emphysema.
 |
| Figure 3: Zephyr (second generation) endobronchial one–way valve. |
A new generation of EBV is ready and is currently under evaluation in a multicenter prospective trial: the Zephyr endobronchial valve (Figure 3). This new valve is a device incorporating a one–way valve supported by a stent–like self–expanding retainer that secures the EBV in place during all physiological conditions, including coughing. The retainer is a self–expanding tubular mesh structure that is cut from Nitinol superelastic alloy tubing and processed to its final expanded dimensions. It is covered with silicone in order to create a seal between the implant and the bronchial wall; the silicone membrane is formed integrally with the struts of the self expanding retainer component. When the EBV is delivered into the target bronchus, the retainer expands to contact the walls of the lumen. This valve has also been designed to allow air to be vented from the isolated lung segment while preventing air from refilling the isolated lung area during inspiration: it vents during expiration and closes when flow is reversed during inhalation. The Zephyr EBV is provided in two sizes: the EBV 4.0 designed for bronchial lumens with diameters of 4.0 mm to 7.0 mm, and the Zephyr EBV 5.5 is designed for bronchial lumens with diameters of 5.5 mm to 8.5 mm. The previous version of the device, as mentioned before, was provided in three different sizes for the same overall treatable lumen diameter range of 4.0 to 8.5 mm.
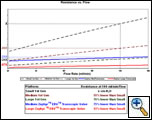
The physical performance of the valve is different according to the type of valve (first generation vs. second generation of EBV), and varies according to the size of the device itself. In other words, the opening pressure, and thus flow resistance, was higher for the EBV of the first generation when compared to the Zephyr valve. On the other hand, within the two different models of valves, flow resistance is lower for valves having a larger diameter. Overall, expiratory air flow is much higher for large valves of the second generation (Figure 4).
A flexible delivery catheter is used to place this second generation EBV valve into the targeted bronchial lumen. The catheter is constructed of a flexible stainless steel and polymer composite shaft. It has an actuation handle (Figure 5) on the proximal end and a retractable polymer housing for containing the compressed Zephyr EBV on the distal end (Figure 6). A bronchial diameter measurement gauge made of flexible polymer is attached to the proximal end of the distal housing (Figure 6). This measurement gauge allows the user to visually (bronchoscopically) measure the diameter of the bronchial lumen prior to device deployment to verify that the size of the valve is appropriate for the target lumen. The measurement device consists of two sets of flexible gauges. On the delivery catheter for the Zephyr EBV 4.0 the larger gauge spans a 7 mm diameter and the smaller gauge spans a 4 mm diameter, indicating the maximum and minimum treatable bronchial diameters for this size of device. On the delivery catheter for the Zephyr EBV 5.5, the two gauges are sized to span diameters of 8.5 mm and 5.5 mm. The EBV is compressed into the retractable distal housing by the operator using a specifically designed EBV loader system. The loaded catheter is advanced to the target location and the valve is deployed by actuating the deployment handle, which retracts the distal housing and releases the EBV. The delivery catheter is designed to be inserted through a 2.8 mm diameter working channel of a flexible bronchoscope. Thus, this new generation of valves can be placed under local anaesthesia since the deployment maneuver is much simpler.
 |
 |
| Figure 5: Handle of the deployment system designed for the second generation of valves (Zephyr EBV). | Figure 6: Distal end of the deployment system for the Zephyr EBV (see text for description) |
After a series of animal experiments, more than 100 patients have been treated so far in pilot studies performed at several centers worldwide, with selection criteria similar to those for LVRS. The inclusion criteria in these pilot studies were similar to those for surgical lung volume reduction: heterogeneous emphysema, FEV1 less than 30%, CLCO higher than 20%, no pulmonary hypertension, no hypercapnia. Heterogeneous emphysema was chosen since this type of disease shows less collateral ventilation that the homogeneous one; thus, it should be easier to achieve volume reduction and even atelectasis. The first series of patients treated with a first generation type of EBV were reported by Snell and colleagues [6]. They demonstrated that that type of bronchoscopic prosthesis could be safely and reliably placed into the human bronchi; however, symptomatic improvement was observed only in 4 patients, with no major change in radiographic findings, lung function, or 6 minute walk distance at one month, although gas transfer improved from 7.47 ± 2.0 to 8.26 ± 2.6 ml/min/mmHg and nuclear upper lobe perfusion fell from 32 ± 10 to 27 ± 9 %. Toma and colleagues subsequently reported on 8 patients [5] undergoing unilateral volume reduction with a second generation of EBV. Five patients had emphysema judged too severe for volume reduction surgery and 3 refused the operation. After valve placement there was a 34% increase in FEV1 and 29% difference in DLCO; CT scans showed a substantial reduction in regional volume in four of the eight patients. The same group also reported that in a subgroup of patients in whom invasive measurements were performed, improvement in exercise capacity was associated with a reduction of lung compliance and isotime esophageal pressure–time product [9]. Other two series of patients treated with EBV have been reported [7, 8] with encouraging functional results. Along with the functional improvement there was also a subjective improvement benefit reported by most of the patients, even if a dyspnoea score was not available in all the series. Overall, all patients tolerated the treatment well. Between 3 and 5 valves were placed in the target lobe and most of them received unilateral treatment. It has been demonstrated that the procedure can be safely performed with encouraging short–term results. Up to now the data available for this technique are still extremely limited and the follow–up is too short to be compared with other therapies.
In our experience [8] with the first generation of EBV valves we have observed 1 contralateral and 2 bilateral pneumothorax out of 17 treatments (2 staged bilateral); this complication has been experienced also by other authors [7]. However, with the second generation of EBV valves (5 patients – unpublished data) we have not observed this complication any more. Three of our patients showed granulation tissue obstructing one or more of the valves; this complication occurred with the first generation valves 6 months after placement. One patient had pneumonia in the non treated lobe; this complication was easily managed with the administration of broad spectrum antibiotics. The functional improvement was statistically significant; in particular FEV1 markedly improved and the residual volume decreased: at 3 months more than 50% of the patients still show at least a 30% functional improvement; most of them required less supplemental oxygen and 7 out of 15 were able to stop it. We were not able to observe a complete atelectasis of the lobe where valves where implanted, even if it has been described by other authors; however, in most of the patients, the shape of the chest was redesigned. Exercise tolerance was also improved and remained stable after 3 months of follow up. Contralateral BLVR could be attempted to obtain a second functional improvement when pulmonary function tests start to deteriorate again, as it is done for LVRS. A contralateral BLVR was performed in two of our patients, but neither was required for functional reasons: both patients had pneumothorax on the contralateral side and valves were placed with the aim of stopping the air leak; this result was easily obtained, along with further functional improvement. With more experience, simultaneous bilateral insertion of the valves could be attempted. One of the advantages of the endobronchial lung volume reduction is that the procedure can be reversed and other treatments tried if necessary.
The short term results with BLVR are encouraging, but long term follow up is certainly required, as well as multicenter trials, to evaluate the therapeutic potential of this procedure.
References
- Lausberg HF, Chino K, Patterson GA, Meyers BF, Toeniskotter PD, Cooper JD. Bronchial fenestration improves expiratory flow in emphysema human lungs. Ann Thorac Surg 2003;75:393–397.
- Rendina EA, De Giacomo T, Venuta F, et al. Feasibility and safety of the airway by pass procedure for emphysema. J Thorac Cardiovasc Surg 2003;125:1294–1299.
- Choong CK, Haddad FJ, Gee EY, Cooper JD. Feasibility and safety of airway bypass stent placement and influence of topical mitomycin C on stent patency. J Thorac Cardiovasc Surg 2005;129:632–638.
- Fann JI, Berry GJ, Burdon TA. Bronchoscopic approach to lung volume reduction using a valve device. J Bronchol 2003;10:253–259.
- Toma TP, Hopkinson NS, Hiller J, et al. Bronchoscopic lung volume reduction with valve implants in patients with severe emphysema. Lancet 2003;361:931–933.
- Snell GI, Halsworth L, Borrill ZL, Thompson KR, Kalff V, Smith JA, Williams TJ. The potential for bronchoscopic lung volume reduction using bronchial prosthesis: a pilot study. Chest 2003;124:1073–1080.
- Yim AP, Hwong TM, Lee TW et al. Early results of endoscopic lung volume reduction for emphysema. J Thorac Cardiovasc Surg 2004;127:1564–1573.
- Venuta F, De Giacomo T, Rendina EA, et al. Bronchoscopic lung volume reduction with one way valves in patients with heterogeneous emphysema. Ann Thorac Surg 2005;79:411-6.
- Hopkinsons NS, Toma TP, Hansell DM, Goldstraw P, Maxham J, Geddes DM, Polkey MI. Effect of Bronchoscopic lung volume reduction on dynamic hyperinflation and exercise in emphysema. Am. J Crit Care Med 2005;171:423–424.