ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Repair of an Anterior Postinfarction Ventricular Septal Rupture by the Technique of Infarct Exclusion
Patient Selection
One of the most devastating complications of myocardial infarction is postinfarction ventricular septal rupture. The incidence is approximately 1-2% after acute myocardial infarction.1, 2 The majority of cases involve the anteroapical septum secondary to occlusion of the left anterior descending artery. In the minority, occlusion of a dominant right coronary artery or a dominant left circumflex artery feeding the posterior descending artery results in posterior septal rupture. Patients are usually discovered to have a loud holosystolic murmur in association with clinical deterioration and right-sided heart failure 2-5 days post-infarction.3, 4
There are two standard methods of repair. The first involves using a prosthetic or pericardial patch to cover the defect by suturing the patch circumferentially to the septum. The two major drawbacks of this method are that a) the sutures may be placed through ischemic, friable muscle and tear, and b) the ventriculotomy (which is usually made through the zone of infarct) is subject to LV systolic pressures after surgery.
To avoid these potential problems, David described a method of infarct exclusion that creates a neo-left ventricle using a pericardial patch.5 The septal defect, septal infarction, and free wall infarction (if present) are all excluded from the high pressures of the left ventricle.
Operative Steps
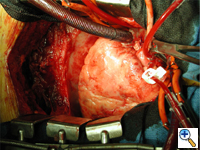
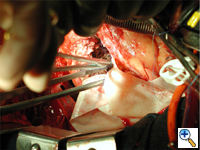
A transesophageal echocardiogram probe should be available in the OR so the repair can be inspected upon completion. The patient is given general anesthesia and prepped and draped in the standard fashion. A median sternotomy is performed and if concomitant coronary artery bypass is planned, the internal mammary artery may be dissected at this point. Otherwise, the pericardium is opened and the heart inspected for evidence of transmural infarction. Single or double venous cannulation can be used, with standard aortic cannulation and full cardiopulmonary bypass is begun (Figure 1).
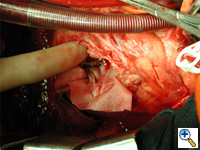
If coronary artery bypass grafting will also be performed, the grafts are sewn first (in this case, internal mammary to left anterior descending) (Figure 2).
 |
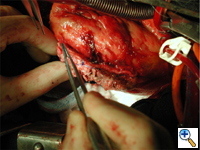 |
| Figure 1. | Figure 2. |
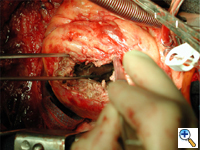
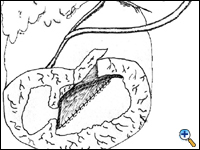
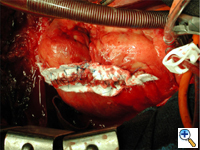
An anterolateral left ventriculotomy is made through the area of infarction parallel to and two centimeters away from the left anterior descending artery. Stay sutures can be placed through the edges of the ventriculotomy to maintain an open visual field. The interventricular septum, area of infarction, and site of rupture are visualized (Figure 3).
The necrotic portion of the septum is inspected but no debridement is necessary. The defect is not closed rather it is excluded from the ventricular cavity (Figure 4).
 |
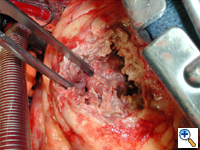 |
| Figure 3. | Figure 4. |
A patch of bovine pericardium is brought onto the field and first sewn to the basal and posterior septum behind the defect using 3-0 polypropylene in a continuous running fashion. Sutures must be placed far from the infarct in healthy muscle. With posterior or extensive infarcts it may be necessary to sew the patch into the mitral annulus. Sutures must be deep with a big needle. Sutures should be firmly pulled up to remove the slack but not excessively so inadvertently cutting through the muscle. A second row of sutures can augment the first. This suture line is meant to hold the patch in place rather than being water tight. This suture line is often easier to perform from the patients left side. This same suture line is continued along the inferior and and anterior walls of the septum to the ventriculotomy (Figure 5).
The patch is then sewn with full thickness sutures to the anterolateral ventricular free wall (the left side of the ventriculotomy) beyond the area of infarction, carefully avoiding the muscle (Figure 6).
 |
 |
| Figure 5. | Figure 6. |
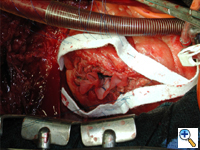
This completes closure of the left ventricular chamber excluding the defect and infarcted septum and ventriculotomy from the high pressures generated by the left ventricle (Figure 7 and 8). It very important that the patch be very floppy and redundant so that it is pushed up against and buttressed by the septum during systole. If the patch is too taut excessive tension will be placed on the sutures and they will rip out.
 |
 |
| Figure 7. | Figure 8. |
Excess patch is trimmed off and the ventriculotomy is closed using Teflon strips sewn onto the ventricular wall using interrupted full thickness horizontal mattress sutures of 3-0 polypropylene (Figure 9).
The sutures are then tied, closing the ventriculotomy (Figure 10). This first row of sutures reapproximates the muscle and secures the Teflon to it. As second double running layer baseball stitch is placed incorporating the Teflon strips and upper muscle layers to provide strain relief and seal gaps. This suture line rarely bleed because it is subject to low right sided pressures rather than high left sided pressures.
 |
 |
| Figure 9. | Figure 10. |
The transesophageal echocardiogram is now used to assess LV contractility, document that the mitral valve closes normally, and inspect the repair for leakage. Right atrial and pulmonary artery saturations are simultaneously drawn for comparison to assure a step up in the oxygen saturation of less than 5 percentage points. The patient is then weaned from cardiopulmonary bypass. Pacing wires are placed. The sternum, subcutaneous tissues, and skin are closed in standard fashion.
Tips & Pitfalls
- All sutures along the septum must be placed into healthy, nonischemic muscle to avoid the complication of suture line breakdown and a recurrent defect.
- If the muscle along the septum is thin, interrupted sutures with Teflon pledgets may create a stronger repair that will not unravel if one suture erodes through friable muscle.
- Direct closure of the septal defect prior to patch on-lay adds no strength to the repair and distorts the natural geometry of the left ventricle.
- Incising the left ventricle through the area of infarction, and then suturing the patch beyond the infarctotomy, excludes both the defect and the infarction from high left sided pressures.
- We recommend concomitant coronary artery bypass grafting, as it has been shown to improve long-term survival after postinfarction ventricular septal rupture.
- Redundancy of the patch is key as the sutures hold the patch in place, buttressed by the septum. If the patch is stretched taut excessive stress on the sutures might pull them through the fragile muscle.
References
- Hutchins GM. Rupture of the interventricular septum complicating myocardial infarction: pathological analysis of ten patients with clinically diagnosed perforation. Am Heart J 1979;97:165-9.
- Lundberg S, Sodestrom J. Perforation of the interventricular septum in myocardial infarction: a study based on autopsy material. Acta Medica Scand 1962;172:413-7.
- Mann JM, Robert WC. Acquired ventricular septal defect during acute myocardial infarction: analysis of 38 unoperated necropsy patients and comparison with 50 unoperated necropsy patients without rupture. Am J Cardiol 1988;62:8-12.
- Kitamura S, Mendez A, Kay JH. Ventricular septal defect following myocardial infarction: experience with surgical repair through a left ventriculotomy and review of the literature. J Thorac Cardiovasc Surg 1971;61:186-90.
- David TE, Dale L, Sun Z. Postinfarction ventricular septal rupture: repair by endocardial patch with infarct exclusion. J Thorac Cardiovasc Surg 1995;110:1315-20.
- Muehrcke DD, Daggett WM, Buckley MJ, et al. Postinfarct ventricular septal defect repair: effect of coronary artery bypass grafting. Ann Thorac Surg 1992;54:876-80.



