ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Stentless Xenograft Aortic Valve Replacement: Subcoronary insertion of the Toronto SPV valve
Patient Selection
Patient Selection, Rationale for Use and Types of Valves
All patients with aortic valve disease who are candidates for aortic valve replacement with stented tissue valves.
For patients who are candidates for aortic valve replacement with stented tissue valves, stentless xenograft valves have several advantages over the traditional stent mounted tissue valves. Notably, stented xenograft valves are intrinsically obstructive due to the space occupied by the stent and sewing ring. For a given external diameter, the internal diameter of the stentless valve is 2 to 4 mm larger than a stent mounted xenograft valve due to lack of a stent. This translates to an ability to place a bioprosthesis with a greater effective orifice area and reduce mean transvalvular gradients.
An increased understanding of the functional anatomy of the aortic root has reinforced the concept of the dynamic relationships among the valve cusps, annulus, sinus of Valsalva, and sinotubular junction. The use of a stentless valve maintains these interactions resulting in improved hemodynamic performance. Recent studies show that the use of stentless xenograft valves has resulted in lower mean transvalvular gradients and a greater reduction in left ventricular mass than stented valves. Early data shows a trend towards improved long term survival in stentless valves.
Implantation of a stentless xenograft aortic valve is technically more difficult than a stented valve but easier than an allograft used in the subcoronary position. Two valves approved for use by the United States Food and Drug Administration are the Toronto SPV (St. Jude, Minneapolis, MN) and the Freestyle valve (Medtronic, Minneapolis, MN). The Toronto SPV is comprised of the valve and supporting aortic wall only, and is designed as a subcoronary implant. The Freestyle valve is a root xenograft that may be used for either a subcoronary, cylindrical or a root replacement implant.
Operative Steps
Preference Card
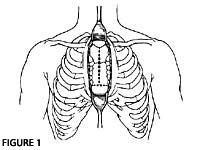
- Set up for standard aortic valve replacement including left ventricular venting.
- Have coronary ostial cannula available for antegrade cardioplegia.
- Sutures include 3-0 or 4-0 Ticron with a RB-1 needle for the proximal suture line, 4-0 polypropylene with a RB-1 needle for the distal suture line, and 4-0 polypropylene with a SH-1 needle for the aortotomy closure.
Tips & Pitfalls
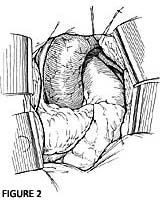
- Avoid opening the aorta too proximal to the sinotubular junction. This leads to technical difficulty in closing the aorta, as the valve posts will extend beyond the aortotomy.
- As with any aortic valve replacement, complete debridement of the diseased aortic valve, annulus and distal suture line is imperative.
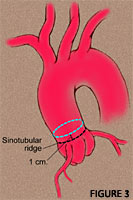
- Selection of stentless valve size is based on the sinotubular junction and annular diameters. The larger of the two diameters is the appropriate size as long as the diameters are within 10% of each other.
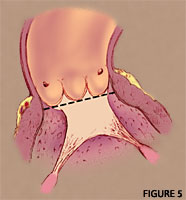
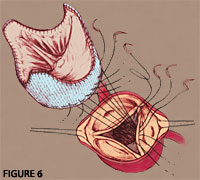
- The muscular portion of the stentless xenograft valve should be aligned with the non-coronary cusp region.
- The proximal suture line is placed in the sub-annular position as a single horizontal plane.
- Suture bites in the muscle below the commissure between the right and noncoronary cusp should be shallow to avoid the Bundle of His.
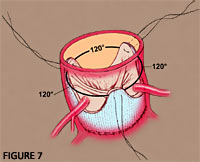
- Be sure valve posts are 120° apart, the same height and not twisted.
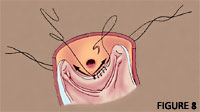
- Keep 2 to 4 mm away from the coronary ostia.
References
- Reardon MJ, David TE. Stentless xenograft aortic valves. Curr Opin Cardiol 14: 84-89, 1999.
- David TE, Puschmann R, Ivanov J, Bos J, Armstrong S, Feindel CM, Scully HE. Aortic valve replacement with stentless and stented porcine valves: a case-match study. J Thorac Cardiovasc Surg 116:236-41, 1998.
- David TE, Feindel CM, Scully HE, Bos J, Rakowski. Aortic valve replacement with stentless porcine aortic valves: a 10-year experience. J Heart Valve Dis 7(3): 250-254, 1998.
- Reardon MJ, Conklin LD, Philo R, Letsou GV, Safi HJ, Espada R. The anatomical aspects of minimally invasive cardiac valve operations. Ann Thorac Surg 67: 266-68, 1999.