ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Approximation of Scimitar Vein to Atrial Septal Defect During Scimitar Syndrome Repair
Kilcoyne MF, Do-Nguyen CC, Moulick A, Mahan V, Mesia CI, Stevens RM. Approximation of Scimitar Vein to Atrial Septal Defect During Scimitar Syndrome Repair. April 2020. doi:10.25373/ctsnet.12104028
Introduction
Scimitar syndrome is a rare congenital disease characterized by lung hypoplasia and anomalous pulmonary venous return from the right lung to the inferior vena cava (IVC) or right atrium (RA). This anomalous pulmonary vein is referred to as the scimitar vein (SV). Without surgery to correct this left-to-right shunt, many patients are at risk of right ventricular failure and pulmonary hypertension (1). While the benefits of surgical intervention have been demonstrated, the optimal surgical technique to avoid complications, such as SV stenosis and baffle obstruction, remains unclear (2, 3).
Patient Background
A 12-year-old boy was born with scimitar syndrome including a solitary SV draining juxtaposed to the right hepatic vein (RHV), a hypoplastic right lung, hypoplastic right pulmonary artery (PA), and large aortopulmonary collaterals (APCs) from the descending aorta to the right PA. The patient presented at 6 months old in significant respiratory distress and underwent transcatheter coil occlusion of the APCs with three vascular plugs, which improved the patient’s symptoms. In longitudinal follow-up, lung perfusion studies at eight months and six years found that right lung perfusion increased from 21.0% and 31.2% of total lung volume, respectively. At 12 years old, cardiac catherization found a Qp/Qs of 2.1 and he was referred for surgical correction of the SV.
Surgical Technique
The patient was taken to the operating room and underwent a median sternotomy. The pericardium was harvested during the sternotomy for augmentation of the atriotomy. The patient was placed on cardiopulmonary bypass, cooled to 22 degrees Celsius, and placed on deep hypothermic circulatory arrest. A vertical right atriotomy was made, which allowed for visualization of the SV orifice draining just superior to the RHV.

Figure 1
An atrial septal defect (ASD) was created and a portion of the septum was resected. Using 5-0 prolene suture, the inferior border of the newly created ASD was approximated to the atrial tissue just superior to the SV. This anastomosis creates the floor of the baffle (Figure 1).
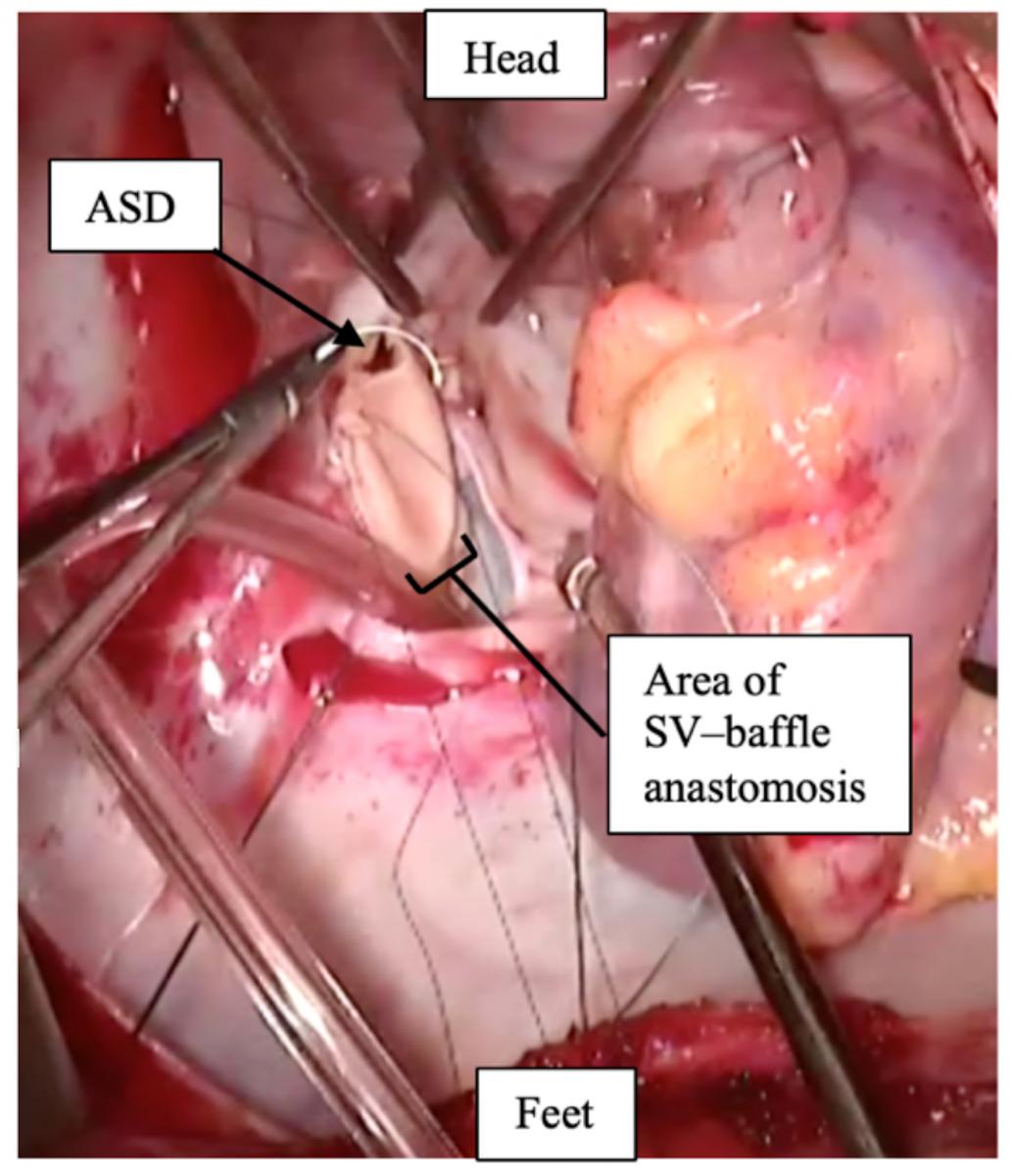
Figure 2
The atrial tissue at the junction of SV and RHV was then sutured to a bovine pericardial patch, creating a baffle. The medial aspect of the baffle was sutured lateral to the coronary sinus and then continued circumferentially to the superior portion of the ASD. This was replicated on the lateral baffle, continuing circumferentially until the atrial baffle successfully allowed for rerouting of SV blood to the left atrium (LA) (Figure 2).

Figure 3
The harvested pericardial patch was then used to augment the area around the right atriotomy (Figure 3).
Follow-up
The postoperative echocardiogram demonstrated no baffle obstruction and low velocity IVC and hepatic vein flow. One year after the surgery, the patient was asymptomatic and an echocardiogram demonstrated unobstructed pulmonary venous return to the LA.
Conclusion
Numerous techniques have been introduced to reroute the SV to the LA. Approximating the ASD to the SV orifice is advantageous because it reduces tissue traction, minimizes anatomical distortion, and creates a wide baffle.
References
- Gudjonsson U, Brown JW. Scimitar syndrome. Pediatric Cardiac Surgery Annual Seminars in Thoracic and Cardiovascular Surgery. 2006;9(1): 56-62.
- Wang H, Kalfa D, Rosenbaum MS, Ginns JN, Lewis MJ, Glickstein JS, et al. Scimitar syndrome in children and adults: natural history, outcomes, and risk analysis. Ann Thorac Surg. 2018;105(2):592-598.
- Vida VL, Guariento A, Milanesi O, Gregori D, Stellin G. The natural history and surgical outcome of patients with scimitar syndrome: a multi-centre European study. Eur Heart J. 2018; 39(12): 1002-1011.
Disclaimer
The information and views presented on CTSNet.org represent the views of the authors and contributors of the material and not of CTSNet. Please review our full disclaimer page here.




