ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Labor-Induced Diaphragmatic Hernia Causing Emergency
Jan A, Awan N, Shah SMA, Khan AM, Rehman S. Labor-Induced Diaphragmatic Hernia Causing Emergency. November 2019. doi:10.25373/ctsnet.10293632.
Introduction:
Any abnormal defect in the diaphragm that may cause protrusion of abdominal contents into the thoracic cavity is known as a diaphragmatic hernia. Diaphragmatic hernias may be congenital or acquired. Acquired diaphragmatic hernias may be traumatic or iatrogenic, while spontaneous diaphragmatic hernias are rare. The authors present the case of a spontaneous acquired diaphragmatic hernia.
Case Summary:
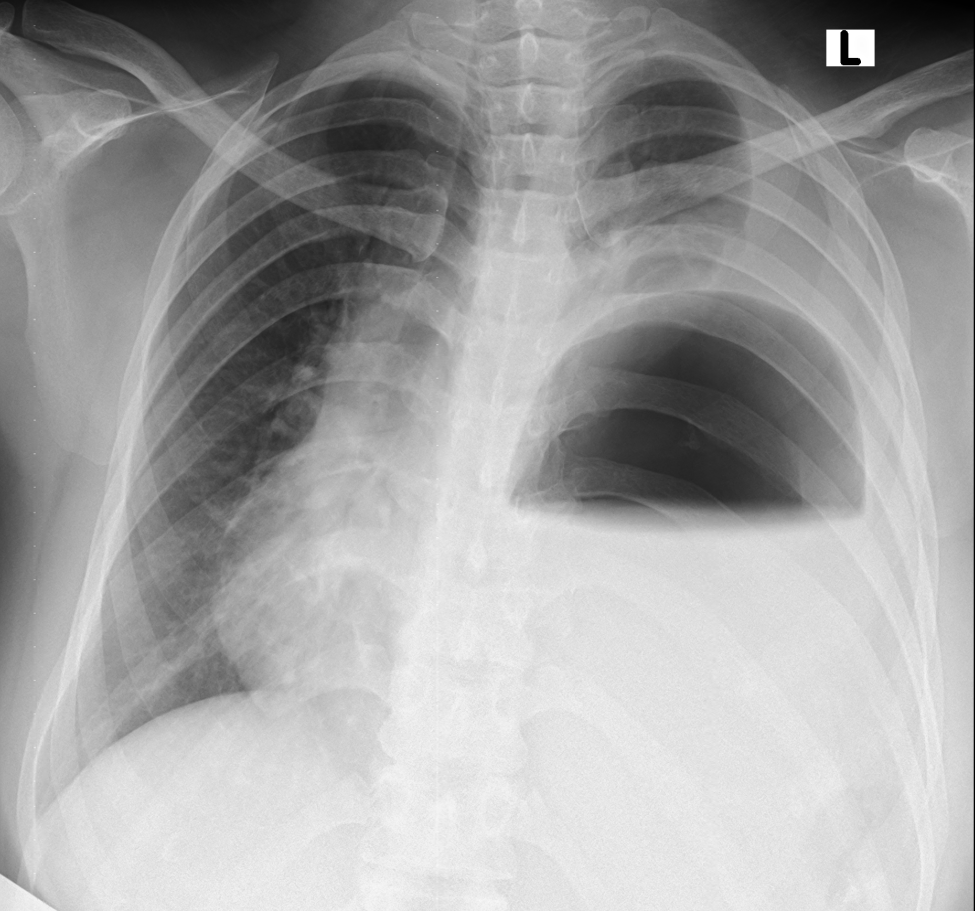
Figure 1. Chest x-ray at arrival showing an air-fluid level in the left hemithorax with contralateral mediastinal shift.
A 27-year-old woman presented to the emergency department with complaints of shortness of breath and cough with sputum for the last three days that had worsened since the morning of presentation. Her history was significant for gestational amenhorrea of 32 weeks. This was her second pregnancy. Her vital signs were within the normal limits. A physical exam revealed absent breath sounds on the left side and a gravid uterus of about 30 weeks. A chest x-ray was done which showed air fluid levels in the left chest with upward pointing meniscus. The authors’ differential included a diaphragmatic hernia, diaphragmatic eventration, hydatid cyst, and loculated empyema. An obstetrician was consulted, and after an examination, they declared that the patient was in labor. She delivered a healthy baby through normal vaginal delivery. After labor, she was comfortably lying in bed with normal vital signs and no active complaints. However, a little later, the patient started to become tachypneic and tachycardiac. Her respiratory rate was more than 50 per minute and heart rate was more than 140 per minute. An electrocardiogram was done which showed sinus tachycardia. She was shifted to the intensive care unit and was intubated for progressing respiratory failure. A nasogastric tube was passed and approximately more than two liters of gastric content was aspirated. An urgent echocardiogram was obtained which showed a right ventricle strain and a dilated Inferior vena cava without respiratory variation. The patient was urgently shifted for a computed tomography of the chest with intravenous contrast, which revealed a large diaphragmatic hernia on the left side. The stomach, omentum, splenic flexure of the colon, the descending colon, small bowel, spleen, and tail of the pancreas were all present in the left chest cavity. There was a mediastinal shift to the right, and the left lung was collapsed. The right lower lobe also showed signs of compression atelectasis.



Figure 2. Contrast enhances the computed tomography scan of the chest. Transverse sections show abdominal contents in the left hemithorax with a collapsed ipsilateral lung. Moderate right-sided pleural effusion was also noted. Note is made of nasogastric tube in the stomach, seen in the left hemithorax. The stomach, descending colon, and omentum can be seen here in the left hemithorax compressing the ipsilateral lung.
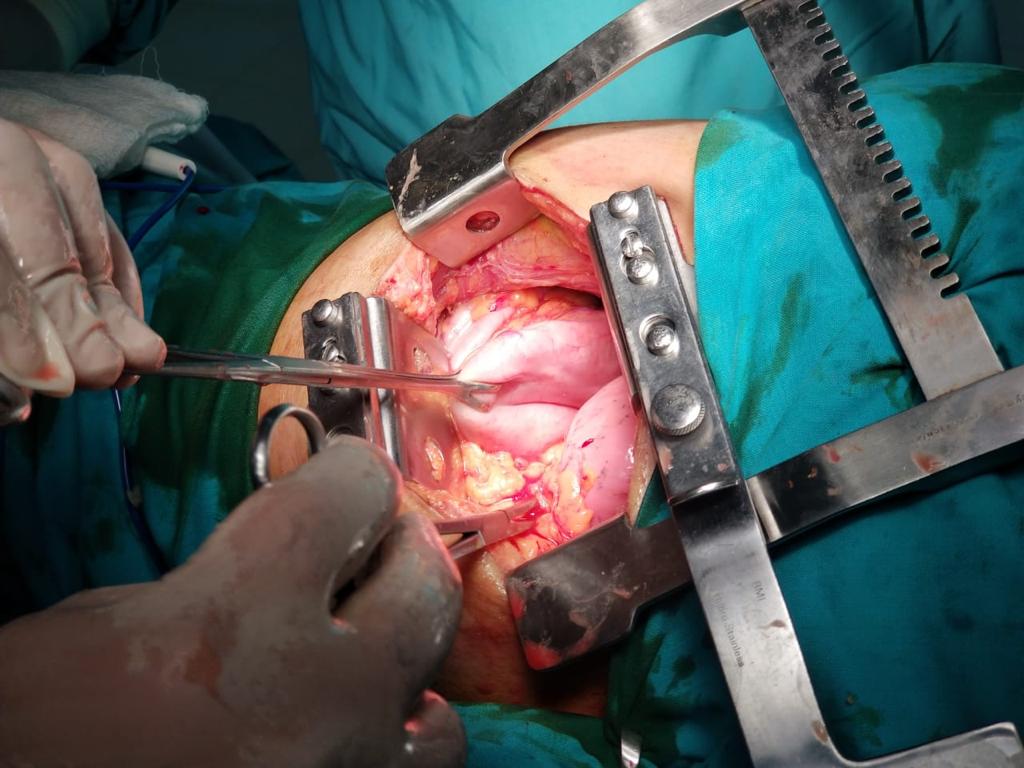
Figure 3. Surgeon's view through a left poetrolateral thoracotomy. Babcock grasping the stomach surrounded by omentum.
The patient was urgently taken to the operation theater and a left posterolateral thoracotomy incision was placed. After dividing the subcutaneous fat and muscle, the seventh intercostal space was entered. Contents of the hernia were visualized in the chest cavity and were manually reduced using digital compression. A loop-shape defect measuring approximately 15 cm in length was identified in the anterolateral part of the muscular portion of the diaphragm. The defect was repaired in three layers using a Prolene® 1 suture in a continuous fashion.
The lung was expanded using valsalva maneuvers. Two chest drains were placed and a routine closure of the chest was performed. The patient was extubated and shifted to the intensive care unit for postoperative care. Twenty-four hours later, she was transferred to the ward. The authors removed the chest drains on the second postoperative day. The patient was discharged home on the third postoperative day. Her postoperative recovery was smooth and uneventful.

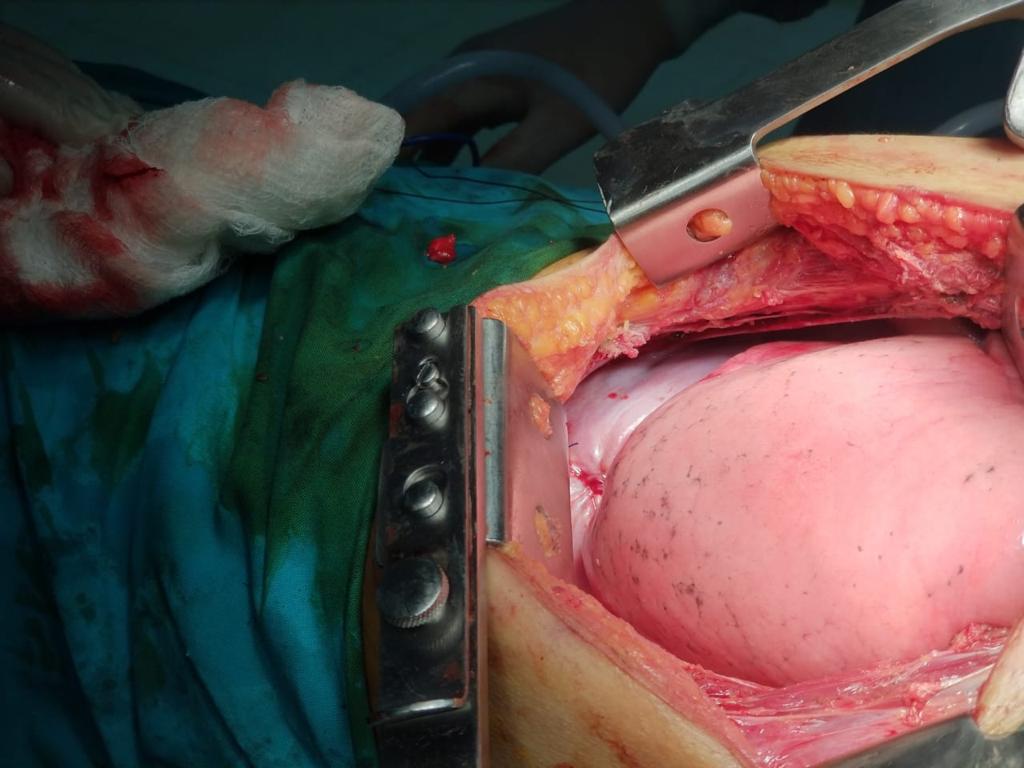
Figure 5. Diaphragmatic defect repaired using Prolene suture in three layers. Lung expanded completely after repair.
Discussion:

Figure 6. Immediate postoperative chest x-ray showing completely expanded left lung. Chest tubes were removed on the third postoperative day.
A diaphragmatic hernia may be acquired or congenital. Traumatic acquired diaphragmatic hernias make up most of all acquired diaphragmatic hernias. Spontaneous acquired diaphragmatic hernias are a rare entity with very few cases reported worldwide. The main mechanism cited behind a nontraumatic diaphragmatic hernia is an increase in intra-abdominal pressure that leads to rupture of the diaphragm. Rushabh Shah, et al, performed a literature review of all cases reported of spontaneous nontraumatic diaphragmatic hernia in which she laid out the following etiological conditions which included: coughing (32%), heavy weight lifting (21%), vaginal delivery (14%), vomiting (7%), and massage in one (4%); no history was available for a single comatose patient. There were five (18%) patients in whom no effort preceded the hernia.
Spontaneous diaphragmatic hernias most commonly occur either at the esophageal hiatus or at sites of impaired development of the diaphragm. In case of the latter, they are found either at the subcostal margin (ie foramen of Morgagni) or posteriorly (ie foramen of Bochdalek).
Diaphragmatic hernias may present in an acute state with signs and symptoms of respiratory distress and/or bowel obstruction. In the authors’ case, the patient was in respiratory distress secondary to gastric outlet obstruction. A simple chest radiograph showing an air-fluid level in the chest within a stomach-like contour will usually aid in diagnosis. This can then be further confirmed by doing a computed tomography of the chest. The stomach should be decompressed with a nasogastric tube to improve symptomatology. In some cases, this may even reduce the hernia. However, definitive management is surgical. This requires the repair of the defect either through the abdominal approach (open vs laparoscopic) or thoracic approach (open vs VATS). In the authors’ case, they did a posterolateral thoracotomy. They found the defect in the anterolateral edge of the diaphragm. Repair of the diaphragm can be performed either by primary closure with direct suturing of the diaphragmatic muscle or in cases where the defect is large and/or the diaphragm is lax and redundant, a polypropylene mesh may be used to strengthen the repair. The authors repaired the diaphragm primarily with prolene suturing continuously in three layers. They found this to be sufficient.
Complications of a diaphragmatic hernia include acute respiratory distress with or without bowel obstruction that may or may not lead to bowel ischemia.
Conclusion:
A labor-induced diaphragmatic hernia is a rare but life-threatening condition that, if diagnosed appropriately, can be managed completely and safely by early surgical repair.
References
- Gupta S, Bali RK, Das K, Sisodia A, Dewan RK, Singla R. Rare presentation of spontaneous acquired diaphragmatic hernia. Indian J Chest Dis Allied Sci. 2011;53:117-119.
- Jangpangi DS, Mrigpuri P, Goyal A, Kulshreshtha VN, Rawat J, Gupta A. Spontaneous diaphragmatic hernia masquerading hydropneumothorax. Indian J Chest Dis Allied Sci. 2017;59;191-193. (available at: http://www.vpci.org.in/uploads/CR-2(5).pdf)
- Shah R, Shah D, Shah M, Patel J. Spontaneous diaphragmatic hernia-a case report and review of literature. SM J Surg. 2017;3(1):1008.
- Stoica SC, Craig SR, Soon SY, Walker WS. Spontaneous rupture of the right hemidiaphragm after video-assisted lung volume reduction operation. Ann Thorac Surg. 2002;74:929–931.
- Darocki MD, Medak AJ. Spontaneous diaphragmatic hernia. Clin Pract Cases Emerg Med. 2018 Aug;2(3):244-246.





