ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Giant Pulmonary Leiomyosarcoma: A Case Report
Sastre I, España M, Ceballos R, Bustos M. Giant Pulmonary Leiomyosarcoma: A Case Report. January 2020. doi:10.25373/ctsnet.11503248.
Case
A 78-year-old woman with a history of rheumatoid arthritis consulted for progressive dyspnea of two months of evolution, associated with asthenia.
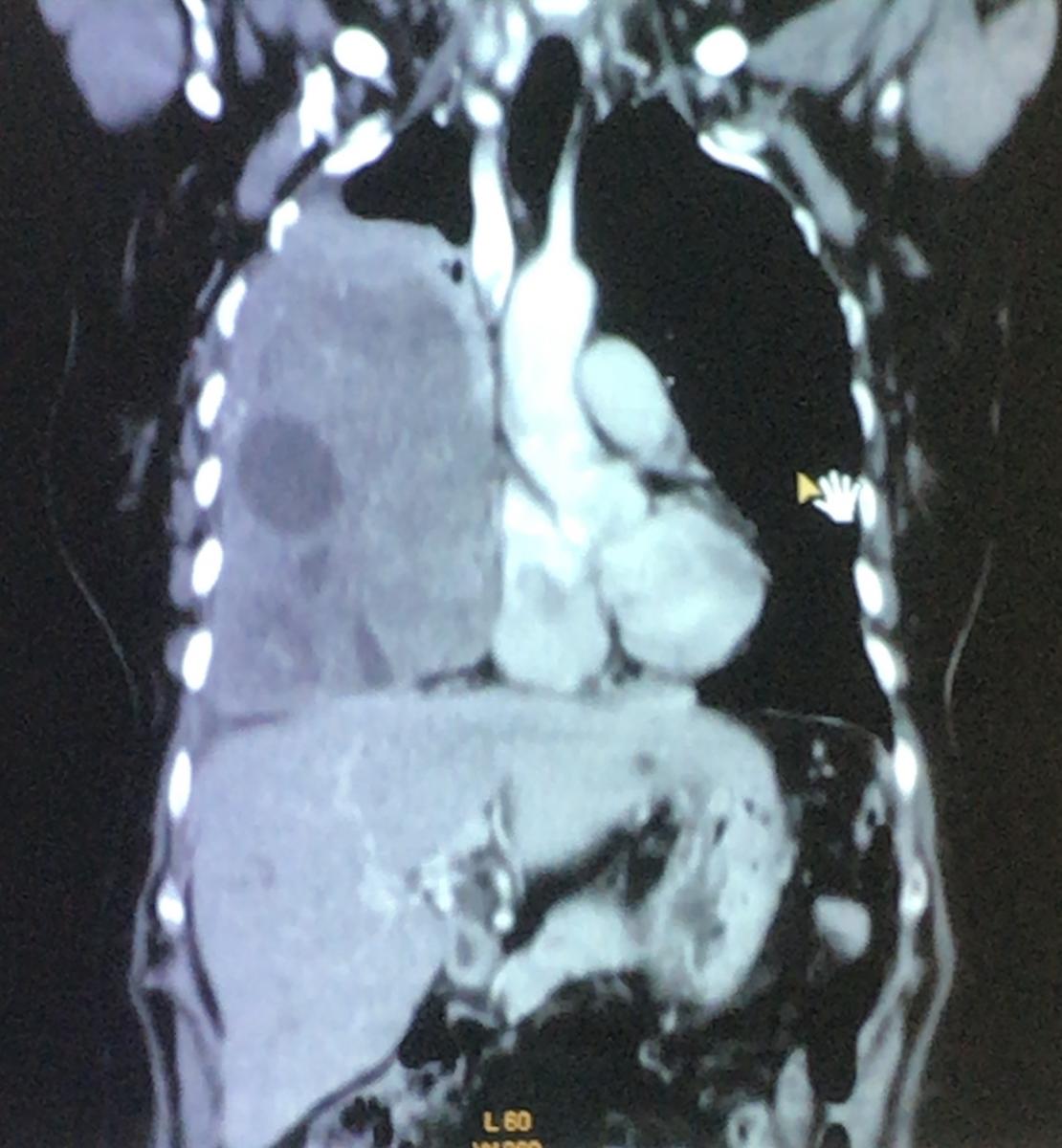
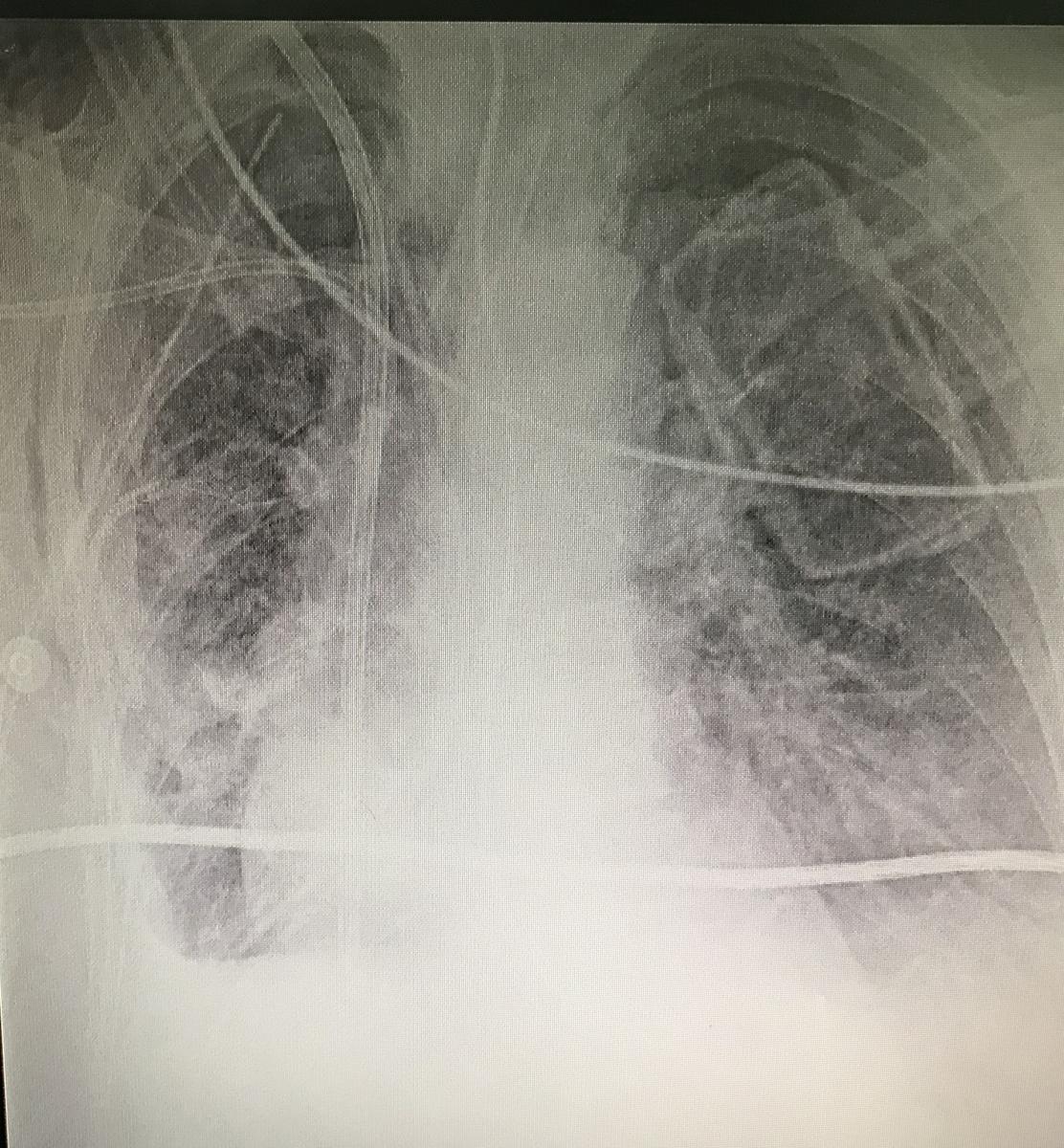
Figure 1. Coronal section of computed tomography, where heterogeneous lesion with cystic area is observed, which displaces the mediastinum, collapses the lung, and flattens the diaphragm.
The physical examination showed the abolition of vesicular murmur in the lower, middle, and part of the upper pulmonary field. She brought spirometry with severe restrictive pattern. Thoracic computed tomography (CT) was performed, where a heterogeneous voluminous mass was observed, with cystic areas, in the right lung, 126 x 166 mm in size, in intimate contact with the thoracic wall, diaphragm, and mediastinal structures (figure 1).
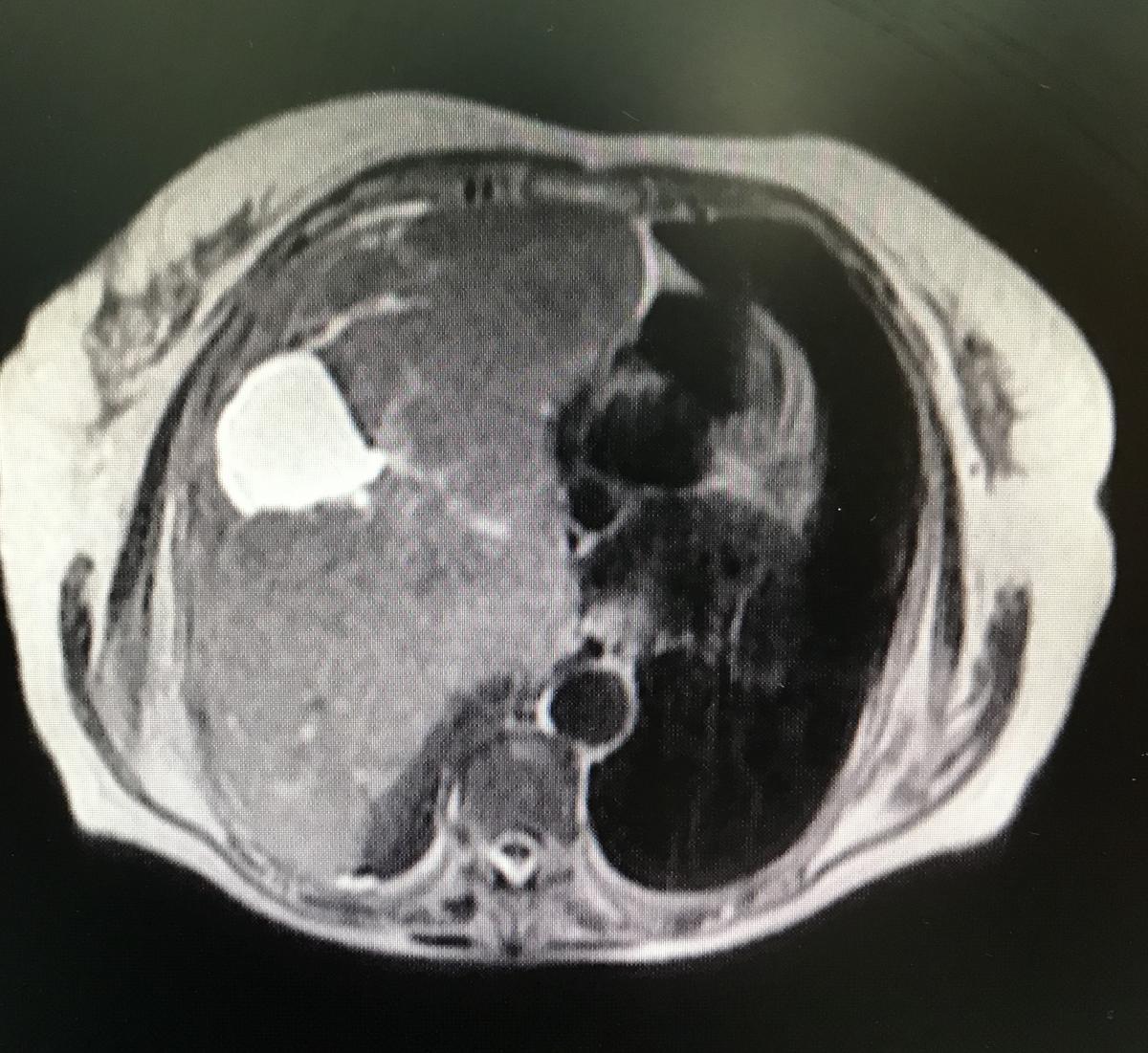
Figure 2. Magnetic resonance, axial section, T2, where the tumor is observed, with cystic areas inside, which compresses without infiltrating adjacent tissues.
Puncion biopsy was performed with trucut. The Pathological Anatomy report is: fusocellular tumor, DC 34 negative, ASMA positive, S 100 negative, NSE negative, Ki 67 2% suggesting low grade leiomyosarcoma as a diagnosis. Magnetic resonance imaging was performed to visualize the presence of infiltration, mainly of large vessels, and studies for distant disease, without finding images compatible with metastasis (figures 2 and 3).
It is decided together with the patient, relatives, and oncology, the surgical behavior to achieve complete extirpation or the greatest possible resection. Videofibrobronchoscopy was performed first, without evidence of endobronchial lesions. The authors continued with a wide right thoracotomy. Complete resection of the tumor was achieved, along with fragment of diaphragm and pulmonary parenchyma. The tumor was approximately 1.5 kg, compatible with low-grade leiomyosarcomade, with lesion-free resection margins (figure 4). The patient achieved good pulmonary expansion in the immediate postoperative period (figure 5). She recovered in the intensive care unit at the beginning, and then continued in the general ward, with good evolution.
Discussion
Lung sarcomas are rare neoplasms representing 0.2-0.5% of all lung tumors, with leiomyosarcoma being the most frequent (1.2). Up to 2015, approximately 127 cases were reported, demonstrating their low frequency. It is more frequent in men (3). It originates in the smooth muscle of the vascular walls of the bronchi, or of the interstitium that surrounds the alveolar walls. Since most of the time it is metastatic, it is necessary to rule out other locations. Clinically, it presents in an unspecified way and can manifest with cough, dyspnea, chest pain, asthenia, or hemoptysis. Early diagnosis is fundamental, since later there are more possibilities of finding metastasis. Computed tomography and magnetic resonance are the studies of choice to assess the morphology of the lesion and local and distant extension in this type of sarcoma (1, 2). The diagnosis is confirmed through biopsy, incisional or excisional biopsy, depending on the size and location of the tumor (2).
Histological diagnosis of leiomyosarcoma is suspected by identifying a fascicular proliferation of spindle cells showing intersections at right angles (1, 3). The use of markers as anti-smooth muscle antibody helps the diagnosis. The applicable therapeutic modalities are surgical resection, radiotherapy, or chemotherapy. Total removal of the lesion is the ideal treatment, as radiotherapy and chemotherapy have not been shown to improve long-term survival. Survival will depend on the grade of the tumor, the size, and the type of resection performed if feasible (1, 2, 3).
In the authors’ case, in spite of the large size of the lesion, the complete surgical resection was achieved with free margins, preserving a good part of the pulmonary parenchyma. In conclusion, the authors believe that a precise preoperative evaluation can lead to a curative surgical treatment, setting aside the paradigm that large lesions are not feasible for resection in the first place. At the same time, the authors contribute this case to the scarce casuistica reviewed in the literature.
References
- Luthra M, Khan H, Maizul Suhail M, Avadhani V. Leiomiosarcoma pulmonar primario: presentación de un caso. Arch Bronconeumol. 2012;48:476–478
- Xie X, Chen Y, Ding C, Yu X, Zou L, Xu B, et al. Primary pulmonary leiomyosarcoma: A case report. Oncol Lett. 2016;11(3):1807–1810.
- Nath D, Arava S, Joshi P, Madan K, Mathur S. Primary pulmonary leiomyosarcoma of lung: An unusual entity with brief review. Indian J Pathol Microbiol. 2015;58:338-340.
Disclaimer
The information and views presented on CTSNet.org represent the views of the authors and contributors of the material and not of CTSNet. Please review our full disclaimer page here.