ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Global Cardiothoracic Surgery Advances and Challenges in Developing Countries and Emerging Economies
Pezzella AT. Global Cardiothoracic Surgery Advances and Challenges in Developing Countries and Emerging Economies. October 2018. doi:10.25373/ctsnet.7247249.
“I am of the opinion that my life belongs to the community, and as long as I live, it is my privilege to do for it whatever I can. I want to be thoroughly used up when I die, for the harder I work, the more I live. Life is no ‘brief candle’ to me. It is a sort of splendid torch which I have got hold of for a moment, and I want to make it burn as brightly as possible before handing it on to the future generations.”
~George Bernard Shaw (1)
Introduction
In 2010, a review of the global aspects of cardiothoracic (CT) surgery summarized the status of CT surgery from clinical, education, research, and administrative points of view (2). The present review expands the discussion to include these and other areas of concern and development.
The maldistribution or underserved areas of CT surgery between countries and within countries is slowly improving. Yet the increase in rural migration to urban areas, as well as population displacement secondary to global wars and climate changes, are hindering the amelioration of this imbalance. The double burden of disease in developing countries or low-middle income countries (LMICs) and emerging economies (EEs) remains an obstacle for the development of increased medical access and care, especially for the increasing noncommunicable diseases (NCDs) and the lingering communicable diseases (CD) (3).
Improved socioeconomic conditions in LMICs and EEs have also witnessed major increases in the need for CT surgical services and procedures for the continuing prevalence of rheumatic heart disease (RHD), the high incidence, prevalence, and backlog of complex congenital heart disease (CHD), and the accelerated increase in coronary artery disease (CAD) and degenerative valve and aortic diseases. As this clinical demand increases, the challenges in LMICs will continue to be access, cost, availability of services, demand for high-tech procedures, qualified health care personnel, and the need for increased quality cardiac care centers.
Currently, technological progress is advancing at a high rate in developed countries. LMICs have lagged behind these advances, and are limited to the standard established open heart operations. This is related to stagnation in the educational structure, the slow or absent evolution of health care policy with regard to cost and access, and the availability of qualified and experienced cardiac centers, CT surgeons, and teams.
To date there is no global database that documents the annual number of CT surgical procedures, their outcomes, the number of trained and certified CT surgeons, or the number of qualified CT surgical teams, hubs, or centers. The seminal work of Unger (4) in 1995 documented the availability of cardiac surgery worldwide. This work has been widely quoted but not updated. There has been a subsequent steady increase in CT surgery globally, but the maldistribution persists.
Globally, CT surgery has morphed into separate disciplines and specialties in developed countries, yet this has happened only slowly in LMICs and EEs. This is reflected in the increasing number of specialized CT procedures listed in the USA Current Procedural Technology® codes and modifiers in developed countries (5, 6).
These advanced procedures include complex neonatal cardiac procedures, minimally invasive adult aortic, mitral, and tricuspid valve repair or replacement, all arterial coronary bypass, off-pump coronary bypass, Maze procedures, heart transplantation, mechanical assist devices, thoracic endovascular aortic/aneurysm repair, transcatheter aortic valve implantation (via trans femoral, caval, carotid, or apical approach), advanced thoracic procedures, especially robotic and video-assisted procedures, minimally invasive esophageal resection and reconstruction, and per-oral endoscopy myotomy. Additional contributions include more efficient anesthesia drugs and methodology, along with improvements in the perioperative care of older high-risk patients.
General thoracic and vascular surgery programs are slowly separating from cardiac surgery in developed countries. In LMICs and EEs, this is not the case. Many CT surgeons there continue to do the full spectrum of the basic open procedures (cardiac, thoracic, vascular, general surgery) that they are capable of performing in order to maintain their surgical skills and supplement their income. Yankah and colleagues (7) evaluated the distribution of 443 cardiovascular procedures in East Africa and the Horn of Africa. Procedures included 63.4% congenital, 23.7% rheumatic valve, 4.5% CABG, and 8.4% other procedures.
Globally, general surgery and the surgical subspecialties have now emerged as essential components of public and global health. The volume of global surgical procedures is increasing, but there remains a dearth of health care resources, especially in CT surgery and other specialties. This is compounded by the high rate of perioperative complications and mortality, especially in sub-Saharan Africa (8).
There is a need to increase the global education and training of future CT surgeons as well as CT surgery teams. The challenges to attract, maintain, and produce quality candidates will require the cooperation of the major CT surgery societies that can organize effective continuing medical education (CME), and international guidelines that provide a framework for competence, experience, confidence, and a broad-based international certificate in the practice of CT surgery. This report highlights these and other areas that have a potential or actual impact on CT surgery.
Background
The interest and knowledge of current world events and activities, geographic changes and events, and world country profiles provides an overview of the global environment we live and work in. This includes basic social, political, economic, environmental, and demographic aspects (SPEED), as well as specific information for any given country, region, or hemisphere (9, 10). It must be appreciated that these five areas are all interrelated with varying levels of direct or indirect importance for and impact on CT surgery.
Sociological Aspects
Sociology is the systematic study of the development, structure, interaction, and collective behavior of organized groups of human beings (11). Huntington (12) has advanced the concept of historical and current global civilizations as a basis to understand the dynamics of current global changes and conflicts. He discusses major and minor civilizations in relation to religion, culture, language, race, and ethnicity (Sinic, Hindu, Islamic, Western, Orthodox, Latin, African, Japanese, Jewish, and Indigenous peoples). Marmot (13) believes that unnecessary disease and suffering of disadvantaged people, whether poor or wealthy, is a result of the way the affairs of society have been organized. He argues that failing to meet the fundamental human needs of autonomy, empowerment, and human freedom is “a potent cause of ill health.”
The syndemics model of health focuses on the biosocial complex (14). This approach to health care initiatives and clinical practice projects conventional historical understanding of diseases as distinct entities in nature, separate from other diseases and independent of the social sector in which they are found. (14).
Political and Governance Aspects
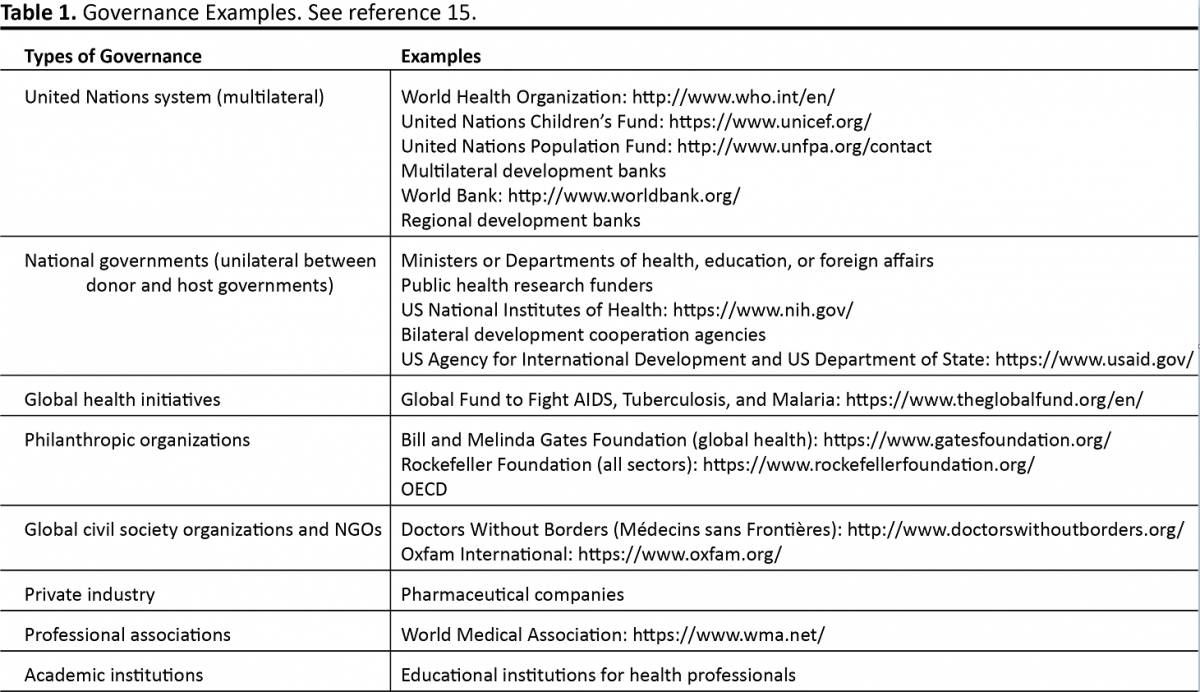
Politics has an important role in all human activity that includes science, arts, health, education, religion, and technology. Politics permeates all the SPEED areas, given its control of laws, rules, and regulations. Eleven political ideological types were identified in the 20th century (12). They included: liberalism, socialism, anarchism, corporatism, Marxism, communism, social democracy, conservatism, nationalism, fascism, and Christian democracy. Governance refers to the ways in which a society organizes and manages its affairs. It includes environment, sustainability, peace and security, human rights, military, and public health. International and national laws and treaties need to be appreciated and understood. All governments and worldwide organizations are involved with varying levels of health care involvement, growth, finance, and development (Table 1) (15). Only the World Health Organization (WHO) has a universal membership and mandate with all the 193 countries in the United Nations (UN), but it has no direct control on any given issue nor is it a source of financial funding. The Organization for Economic Cooperation and Development (OECD) is a major donor that helps governments to increase prosperity and alleviate poverty via economic planning, growth, and financial stability (16).
The governments of all countries are sovereign with regards to laws, rules, and regulations that must be understood and followed (17). As an example, in 2014 Ecuador ruled medical malpractice a criminal offence (18). This became a major issue for local doctors as well as volunteer groups.
In working with foreign countries, it should be stressed that their laws and rules cannot be avoided or bypassed, and they must be understood and followed. Levitsky (19) has nicely adopted the Kissinger term “realpolitik” that places world politics as it really exists, rather than as it is imagined. He further defines it as a proxy for health care based on practical concerns rather than on ethics or theories.
Economic Aspects
The World Bank classification of countries include: low-income (gross national income (GNI) per capita >$1,005), lower-middle-income (GNI per capita between $1,006 and $3,955), upper-middle-income (GNI per capita between $3,956 and $12,235), and high income (GNI per capita of $12,236 or more) (20). The World Bank Group has established two goals for the world to achieve by 2030: (1) end extreme poverty by decreasing the percentage of people living on less than $1.90 a day to no more than 3%, and (2) promote shared prosperity by fostering the income growth of the bottom 40% for every country (20). The World Bank Group is also bent on achieving universal health care coverage by the year 2030.
As noted, the financial support for health care in LMICs and EEs comes from many sources that include individual governments, multilateral, unilateral, corporate, charitable organizations, private sources, self-pay, and combined public/private or philanthropic sources like the OECD (Table 1) (15, 16).
The growth of global cardiac surgery availability parallels the gross domestic product (GDP) (21). GDP is stimulated by free global trade and capital mobility, as well as an increasing global work force that increases wealth creation. The Inverse Care Law, formulated by Julian Tudor Hart in 1971, states: The availability of good medical care tends to vary inversely with the need for it in a population served (22).
Environmental Aspects
The study of geography is divided into physical, human, population, cultural, political, economic, natural resources, and urban or regional areas (23). Current concerns have focused on the dramatic changes in the global environment and climate secondary to natural causes and human activity, as well as the direct and indirect effects on the health of all living things (24).
There have been gradual increases in the annual numbers of deaths, injuries, and diseases due to prevailing changes in the weather and the resultant sequelae that include extreme air pollution, drought, fires, floods, mud slides, hurricanes, desertification, tectonic plate movements (ie, earthquakes, tsunami), volcanos, and eroding coastlines. All of these events need to be understood, appreciated, and placed in a proper perspective with respect to the effects on society and the planet.
Health examples include: direct extension in the geographic range of several vector-borne infectious diseases or their vectors; increases in regional temperatures that may increase coastal outbreaks of cholera relative to the warming of coastal waters and El Niño events; and increases in the cost of staple foods, especially in vulnerable food-insecure regions, which have led to nutritional deprivation in LMICs (25). The interaction of demographics with economic activity and social issues will continue to have both a direct and indirect impact on health-related changes and issues. Global warming is a reality. Debate remains whether human activity is the primary cause or has just accelerated the process. The challenge is what reasonable and rational efforts can and should be promulgated to mitigate these changes and their sequelae.
Demographic Aspects
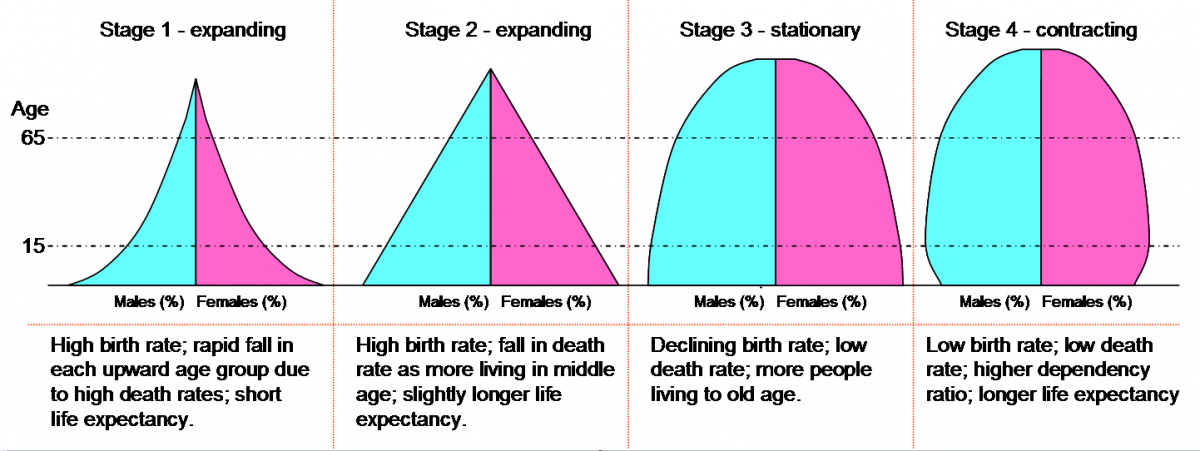
Demographics are the study of populations, especially over time or location. They include the study of the age, size or density, structure, mobility, family structure, and distribution of populations (ie, urban and rural), as well as the changes in response to total fertility rates (TFRs), migration, age, mortality, or disabilities. Demographics also include the study of societies, education, nationality, religion, cultures, and ethnicity (26). The Demographic Transition Model follows the trends of birth and death rates (27). Each stage measures the annual number of births and death rates per one thousand people. As they change, so do social and economic effects on the global population. Figure 1 illustrates the demographic stages with LMICs and EEs at stages 1 and 2, whereas stage 3 is the most common in developed countries. Stage 4 is the most recent trend, where the population growth is at risk. Examples include Russia and Japan with significant declining birth rates and populations.
It is postulated that there are >100 billion humans who have ever lived (28). The global population is presently at 7.5 billion and will grow exponentially to 9.7 billion by the year 2050 in 244 entities, which include countries, territories, colonies, and dependencies, with major growth in LMICs, especially the Sahel and sub-Saharan Africa (28).
The Malthusian theory of population states that technology is growing in a linear or arithmetic fashion and may be unable to keep pace with the growing population that is increasing in a geometric or exponential fashion (29). Yet the increase in population may stimulate the global economies to grow and thus mitigate the effect, especially since by 2050 there will be a 70% increase in the need for food production and an increased and available population to produce it (30).
Applying current technology to decrease global food waste may be a starting point (31). Annual food waste (222 million tons) in developed countries is as high as in LMICs, but in developing countries more than 40% of the food waste occurs after harvest and processing levels, while in developed countries more than 40% of the food waste occurs at discount and retail levels (32).
As noted, TFRs and the live birth rates have decreased in many developed countries like Russia and Japan, whereas the rates continue to increase in LMICs and especially in sub-Saharan Africa (33). Balancing the global population shifts will remain a global challenge.
Globalization
Globalization is not a myth or new phenomenon (34). It is international interaction fueled by increased trade and technological advances, especially over the past 10 years (35). Moore's Law postulates the number of transistors per square inch in an integrated circuit would double every two years. This implies an exponential growth of technology (35). This results in the acceleration of human activity, adaptability, and the interdependence or dependence of many countries.
Basically, the major engine of global activity involves opening national and international borders to allow free trade and fewer tariffs, and to increased flow or transfer, via air, land, sea, and the internet, of three major items. These items include people, products (be they organic or inorganic), and information, knowledge, or finance. Both open and unrestricted trade markets will continue to fuel this globalization. The trend toward nationalism and isolationism is not a viable pathway in this current era of globalization. Levitsky (19) points out that globalization has challenged CT surgery, given that patients can now seek less costly care and surgical operations in LMICs and EEs. This has further created a shift from private practice to a corporate relation and employment system, with doctors now being increasingly involved in hospital or clinic employed relationships.
Mortality
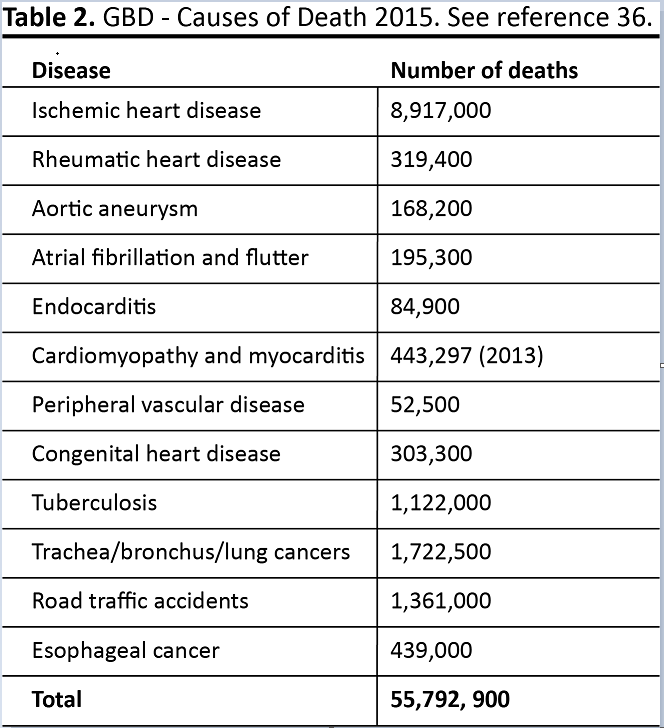
In 2015 there were 55,792,900 global deaths, with 10.5 million among children. The top five causes of death globally were ischemic heart disease (IHD) (7.2 million deaths), stroke (5.5 million), injuries from all causes (4.7 million), lower respiratory diseases (3.9 million), and HIV/AIDS (2.7 million) (36, 37).
The WHO defines three groups of diseases: Group 1, CDs; Group 2, NCDs; and Group 3, injuries. The NCDs are increasing at a higher rate in LMICs and EEs, especially IHD, stroke, chronic obstructive lung disease, and lower respiratory infections.
In 2015 NCDs caused 63% of total global deaths per year, with 80% of those deaths occurring in LMICs. Failure to recognize these diseases in LMICs and EEs, especially the increase in CAD, CHD, and lingering RHD, creates subsequent increases in comorbidity, risk, and complications (Table 2) (3, 36). This has compounded the double burden of disease in LMICs (3). In addition, injuries have become a third category, especially in boys and men 10 to 24 years of age. Road traffic injuries, secondary to increases in autos and poor roads, now fill the hospital beds, with a subsequent drain on hospital services especially the operating room and intensive care unit beds (38).
Disability-Adjusted Life-Years
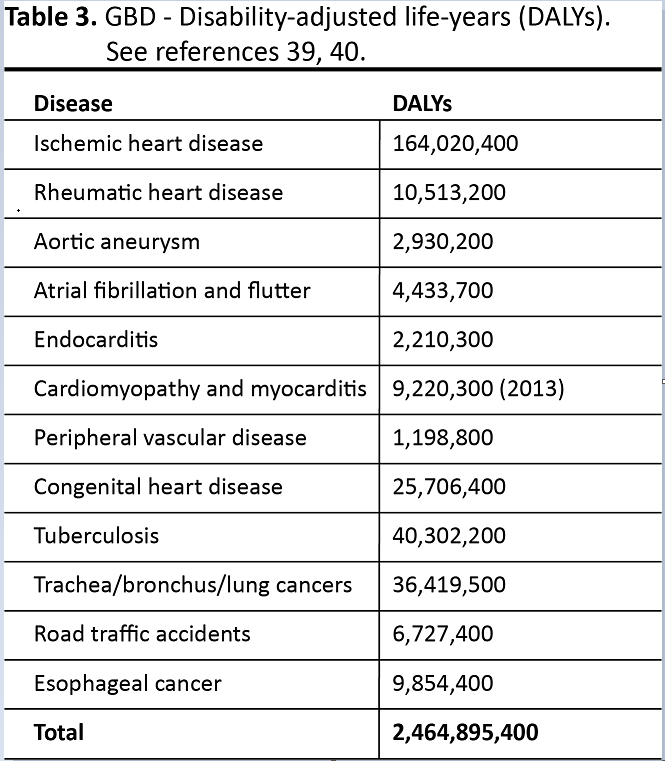
The Global Burden of Disease (GBD) Study has provided an outline to quantify and compare the health of populations by recording both mortality and disability (the disability-adjusted life-year [DALYs]). DALYs are calculated as the sum of the years of life lost (YLL) due to premature mortality in the population and the YLL due to disability (YLD) for people living with the health condition or its sequelae (39). The increase in populations and the average age have offset the DALY gains. Healthy life expectancy (HALE) measures the years lived with a functional health loss before death. The socio-demographic Index (SDI) is a composite of income per capita, average years of schooling, and TFRs.
The leading causes of global DALYs in 2015 included: NCD, 59.7%; CD, 30.1%; and injuries, 10.1%. IHD and stroke rank sixth and seventh as causes of the GBD, followed by road traffic accidents, malaria, and tuberculosis (Table 3) (39, 40). Cardiovascular disease (CVD), cancer, and mental and substance use disorders were among the leading causes of NCD DALYs.
The evaluation of DALYs, HALE, and SDI show that overall global health is improving, yet there is both a trend and increase in functional health loss and subsequent expansion of global morbidity. Increasing personal income, improving education, and decreasing TFRs may mitigate this trend (40).
Human Development Index
A practical metric to monitor the progress of human development or progress is the Human Development Index (HDI). This is a summary measure of average achievement, ranging from 1-100, in three key dimensions of human development: a long and healthy life, being knowledgeable, and having a decent standard of living (9, 41). The HDI is ranked from 0 to100. The highest ranking is Norway at 96.3, and the lowest is Niger at 28.1. The USA is ranked 10th at 94.4.The health dimension is assessed by life expectancy at birth. The education dimension is measured by the mean years of schooling for adults aged 25 years and more, and the expected years of schooling for children of school-entering age. The standard of living dimension is measured by gross national income per capita (42).
The Millennium Development Goals project, supported by 189 UN countries in 2000 and ending in 2015, included three health goals out of its total eight goals. These goals included reduction of child mortality, improved maternal health, and combating HIV/AIDS. Unfortunately, the successor program, Sustainable Development Goals, does not have a defined and focused health care agenda. The only broad-based health-related goal is to “ensure healthy lives and promote well-being for all at all ages” (43). Positive examples include 1 billion people escaping extreme poverty from 1990 to 2015 and the under-five child mortality rate decreasing from 91 to 43 per 1,000 live births over the same time period (44).
Health Care Systems
At present, there is no universal single or multiplayer healthcare system that meets the specific needs and wants of every country. In 2015, 400 million people worldwide had no access to essential health care, and poverty was accentuated by out-of-pocket health care costs (45). Historically, there are four model systems (46):
- Beveridge: Single-payer health care is provided and financed by the government through tax payments. Many, but not all, hospitals and clinics are owned by the government. Some doctors are government employees, but there are also private doctors who collect their fees from the government.
- Bismarck: This model uses an insurance system usually financed jointly by employers and employees through payroll deduction. The health insurance plans have to cover everybody, and they don’t make a profit. Doctors and hospitals tend to be private in Bismarck countries.
- National Health Insurance: This model uses private-sector providers, but payment comes from a government-run insurance program that every citizen pays into.
- Out-of-Pocket: Countries are too poor and disorganized to provide medical care.
These systems vary from a socialistic government payer system with incomplete financial coverage, to a combined public/private insurance system, a total private system, or a system with no or dysfunctional financial support. Globally, access, cost, availability, distribution, and human health resources are not meted out equally given the maldistribution both between countries and within countries (46, 47). Thus there remains a common global need to finance, organize, and develop the health care system in any given country.
Public health is government supported in most countries, given that it benefits the total society and is mandated for the protection of all of its citizens. Yet total health care ranges from public health, preventive self-care and cohort education, to outpatient primary care, in-hospital care, and subsequent continuation of short and long-term surveillance.
In LMICs the government levels of health care are separated between public health and individual curative medical care. Public health argues that it does more for less financial support, whereas curative care requires more financial support for less. The levels of care ascend from the local health clinics to the districts, then the states or provinces, and finally the city or urban hubs. The types of hospitals include government, profit private, charitable trust, military, and special hospitals, like the railway system in India, and military hospitals. Health care costs are government pay, private insurance, charity sources, “self-pay,” and combination initiatives, especially public/private systems.
Leiner (21) proposed a model which places health care and cost in decreasing priorities, with more cost benefits at the lower levels. Level 1 is the higher collective nature with more benefit at less cost. Level 2 and 3 are simple preventive, curative, and emergency issues. Level 4 is complex medical and surgical issues. Level 5 is advanced surgery and high level technology with increased cost for lesser population.
There remains a continuing debate for power, money, and resources between the public health and clinical hospital hierarchies. Within the individual hospital departments there is also competition for financial support, human resources, patient beds, and operating room time. To resolve this impasse requires understanding, cooperation, consensus, compromise, and balance. A balanced approach is warranted that triages those diseases and conditions that require support and priority of care. Covey (48) has nicely described the principle of synergy, which raises compromise, cooperation, collaboration, and congeniality to a higher level and brings about a fresh response that can transform the future.
An organizational and tactical scheme of patient flow is necessary to develop an effective system. The hub and spoke or satellite system can be a very effective system in socialized healthcare systems. It allows an effective direct referral system for complex patient transfers. A recent example is Mexico where regional centers of pediatric cardiac surgery centers will be established to provide more efficient access to needed services (49).
A disease specific horizontal flow model that combines the public health and curative care sectors is also a feasible modality. This practical model includes prevention, education, diagnosis, treatment, rehabilitation, and follow-up monitoring. Again, this requires cooperation, collaboration, consensus, coordination, and transparent communication between the sectors.
Pryor (50) has described an integrated multidisciplinary approach. This provides a more fluid continuity of care. Further, it would improve access, equitability, and availability. It is cost effective, sustainable, accountable, and transparent.
Luckraz and colleagues (51) point out that the initial decision-making process in the management of CAD is the domain of primary care and cardiology. This includes medical management, percutaneous coronary intervention (PCI), or coronary artery bypass surgery (CABG). Currently, there exists a significant worldwide variability in the PCI:CABG ratio that ranges from 2:1 to 8:1 and is very competitive and controversial. Emerging schemes include a decision making process that is carried out with a multidisciplinary team approach.
Blumenfield and colleagues (52), in 2017, noted a decrease in CAD mortality in Israel with the change from physician bias to a “heart team “ concept, as well as decreasing institutional financial pressure on clinical decisions. Towards that end, Molina and colleagues (53) advocate cardiology and cardiac surgery residency programs to include cross-training and rotations on cardiac disease management that includes diagnosis, interventional radiology, interventional cardiology, electrophysiology, and cardiac surgery.
In summary, there is a need for combined cooperative public health and curative care effort, with an emphasis on prevention and individual patient care at the in-patient and out-patient levels. This requires a balance between cohorts, which does more for less, and individual medical care, which does less for more. It also means that medical issues and diseases should be discussed and balanced between simultaneous and sequential pathways. At the medical school level there should be earlier exposure to the public health and curative medicine disciplines. This would inculcate an earlier culture and appreciation of their goals and mindsets.
CT Diseases
As noted, CVD is the most common cause of global deaths and DALYs, especially in LMICs (Table 2). Ten percent of global deaths 100 years ago were secondary to CVD. This has now increased to 30%, with 80% of the CVD deaths occurring in LMICs (54, 55, 56).
Gersh and colleagues (54) have outlined the four stages of epidemiological transition:
- age of pestilence and famine
- age of receding pandemics
- age of degenerative and man-made diseases
- age of delayed diseases, degenerative and NCD
These four stages add support to the theory that NCDs will continue to increase as CDs slowly decrease in LMICs. A fifth stage is proposed in which increased prosperity and urbanization accelerates the incidence of obesity, diabetes, hypertension, and CVD, while social upheaval and economic instability leads to an increase in mortality (54).
The risk factors for CVD include diet, decreased exercise, tobacco use, hypertension, diabetes, increasing alcohol consumption, socioeconomic stress, economic issues, and genetic predisposition (55, 55). The public health preventive measures include cessation of smoking, decrease in salt intake, diet changes, and aerobic exercise. Curative drug measures include lipid reducing agents, blood pressure control drugs, platelet inhibitors, and the polypill (54, 55). Interventions and surgery continue to increase, with PCI growing at a faster rate than CABG (56).
Africa is a major example (57). The incidence of CVD is now the leading cause of death in Africans over 45 years of age. Health care expenditure is 6.3% of GDP, with the government portion only 40% compared to 75% in developed countries. As noted, this is occurring in the setting of the remaining double burden of diseases, and erratic or insufficient government health care spending.
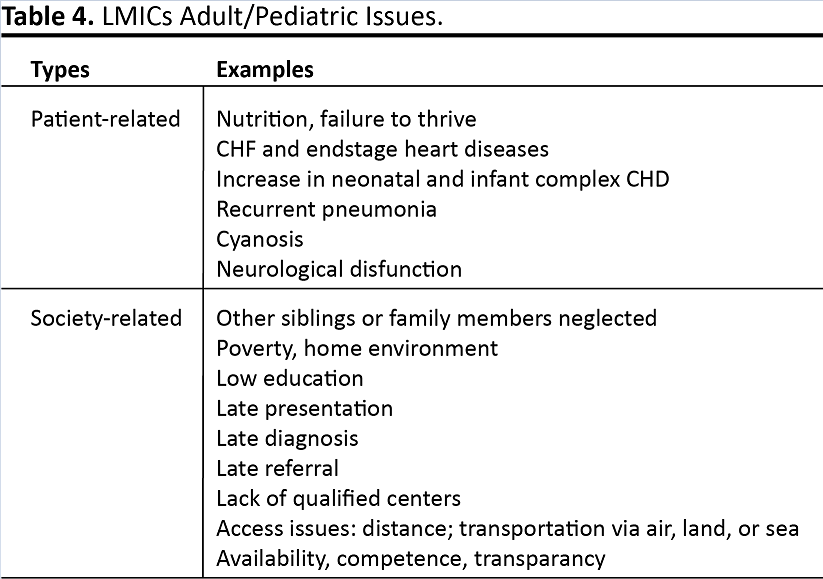
Attention must also be given, in LMICs and EEs, to the increase in CAD, degenerative heart valve disease, lingering chronic RHD, the backlog of CHD that includes an increasing number of complex neonatal and infant groups, and the general thoracic diseases that include trauma (especially motor vehicle accidents), pulmonary tuberculosis, lung cancer, and esophageal cancer. As noted, increased incidence and prevalence, the late referral or recognition, and comorbidity of CHD and RHD compound the need and challenges for increased access and availability of CT surgical care (Table 4) (7, 57-59). These issues can influence the timing and choice of operative procedures that can result in a higher incidence of risk and comorbidity, as well as compounding social issues. One example is rheumatic mitral valve disease in fertile women. There is no consensus regarding the ideal choice of operation, ie, mechanical valve, bioprosthetic valve replacement, or valve repair (60).
Global Health
Global health and governance is a transnational concept and not a specific department, foundation, or business. It has no political authority. It is a concept or strategic action plan with a variety of goals and directions (61). It is designed to promote strategies and goals that can improve global health and equity in worldwide health (61). The major goals of global health initiatives are to support increasing awareness, funding, education, and to improve and advance health care practice, research/development, and overall governance (61). Global health areas include: government health care levels, health education, and department services; nongovernment organizations (NGOs); the corporate private sector; and multilateral or unilateral countries or agencies (Table 1) (15).
The background of global health is rooted in contemporary declarations. Franklin D. Roosevelt, in his State of the Union Message to Congress on January 11, 1944, declared expansion of the Bill of Rights under which a new basis of security and prosperity would be established for all regardless of station, race, or creed. One of the eight bills was health (62):
“The right to adequate medical care and the opportunity to achieve and enjoy good health.”
Later, article 25 of the UN’s Universal Declaration of Human Rights 1948, stated that (63):
"Everyone has the right to a standard of living adequate for the health and well-being of himself and of his family, including food, clothing, housing and medical care and necessary social services."
As stressed, there remains a maldistribution between countries and within countries with regards to access and availability to health care. This involves demographics, cost, and the lingering double burden of disease in the LMICs and EEs. It is clear that there is no comprehensive solution to these causes, but awareness and concern are starting points.
It is doubtful that all countries will witness a government controlled one-payer healthcare system that is totally income free and available in an equitable manor for all of its citizens. The responsibility and cost support for health care in any given country involves the individual, family, government, private sector, and both the employer and employee. Worldwide, public-private partnerships, bilateral agencies, UN agencies, NGOs, and development banks, like the World Bank and OECD, make up the major global organizations in health development assistance. Most of them are independent and have targeted areas of financial health-related support (64, 65).
An effective way to increase global awareness is via education initiatives. Exposing medical students to public health and visa-versa would be a plausible means to increase awareness and participation. Battat and colleagues (66) advocate global competencies that include knowledge or behavior. Examples include the skills to interface with different populations, cultures, and understanding immigration issues.
In the USA, global health has gained interest in affording medical care to disadvantaged populations and decreasing the global maldistribution of health care. Yet there is no international consensus on how this can or should best be accomplished. In the USA there are 133 medical schools, of which 32 (24%) have structured global health activities or programs (67). These include fourth year elective foreign medical rotations and international surgery resident rotations for credit. In the USA there are now global health graduate medical education medical residency tracks. Several USA medical schools and university hospitals have established programs abroad that address medical school education, graduate medical education, patient care, and both clinical and basic research (68, 69). Examples include Duke-NUS Medical University in Singapore (70), Johns Hopkins Medical International (71), and the Cleveland Clinic in Abu Dhabi, UAE (72).
Global Surgery
Global surgery has emerged as an essential component of public health and the global health initiatives (73, 74). It has garnered worldwide attention and support. Maher, in 1980, first addressed the issue of identifying surgery as a necessary and important component of primary health care (70). Global surgery encompasses surgery, anesthesia, nursing, and other health professionals that play a fundamental role in prevention, diagnosis, treatment, and palliation of a broad range of surgical disorders, and are a crucial component of a properly functioning healthcare system.
Farmer and Kim (75), in 2008, pointed out that surgical disease is among the top 15 causes of disability, and accounted for 15% of DALYs. Duda and Hill (76), in 2007, defined global surgery as a treatment or prevention, and further, a surgical condition that is either procedure-oriented or patient-oriented.
The Lancet Commission on Global Surgery, in 2015, reported that 5 billion people, or 70% of the world population, lacked access to safe, affordable, and timely surgical care (77-79). In addition, there was consensus that there remains a substantial global gap between surgical need and the equitable provision of safe surgical care. Unfortunately, a true and accurate estimate of the annual global number of cardiac surgical procedures is difficult to obtain, as is the number of qualified CT surgeons or the number of centers/hospitals that perform cardiac surgery.
There are five areas of global surgery that warrant attention: annual volume, emergence of surgery as a component of public health care, human resources education and training, increasing the quantity and quality of surgery, and innovative plans to fund surgical procedures (80, 81) Further, 143 million additional surgical procedures would be needed to meet the minimum global needs. This would require 1.25 million additional surgeons, anesthetists, and obstetricians.
Weiser and colleagues (80), in 2008, obtained surgical data from 56 countries (29%) among 192 WHO member states. They performed 234.2 million major surgical procedures per year. The rate of surgery included 295 procedures per 100,000 population per year in LMICs versus 11,110 per 100,000 population per year in middle income countries (MICs). The later, with 30.2% of the world population provided 73.6% of the global financial spending in 2004.
Rose and colleagues (81) estimated that 321.5 million surgical procedures would be required to serve the global population of 6.9 billion in 2010. The extremes of range of need were 3,383 operations per 100,000 in Central America, and 6,495 operations per 100,000 in western sub-Saharan Africa. The global need for CVD procedures was 12.1 million.
Shrime and colleagues (82), in 2015, reported that global self-pay surgical care could result in catastrophic costs. This is true for 81 million people each year, be it from the cost of surgery alone or from the medical and non-medical associated costs.
There clearly remains a need to increase the quality of surgical care in developing programs and to decrease perioperative morbidity and mortality (8, 83, 84). Even small efforts can be effective. Examples include the WHO surgical safety checklist (85) and the Surgical Care at the District Hospital manual (86).
Voluntary Humanitarian Efforts and NGOs
Voluntary and humanitarian surgery in poor foreign countries has a long history (87). Over the past 40 years, cardiac surgery oriented NGOs have been involved with developing programs, especially pediatric cardiology and cardiac surgery. As noted, the growth and developments of CT surgery in LMICs and EEs continues to increase as their individual economies grow (22). Table 5 lists 10 regions within three time zones. Regions 2, 5, 6, and 9 are the most needful. There are five types of cardiac centers worldwide: upscale, lateral, upgrading, restarting, and “de novo.” The later three levels are the most involved with NGOs, with level 5 being the most difficult and demanding to initiate and support.
Contemporary activity has included patients coming to developed centers for free or discounted operations; short-term visiting professors from developed programs going to developing countries to give lectures and demonstrate operative techniques; military hospitals doing charity civilian care in war torn areas; local doctors and staff members going to developed programs for short term observation, for nonaccredited 6-12 month fellowships, or for specific areas of training; and donor NGO teams from developed countries with projects in host LMICS and EEs.
Presently, the majority of international NGO programs are involved primarily with pediatric cardiac diseases (88, 89) (Appendix 1). There are fewer NGOs involved with primarily adult cardiac and general thoracic disease care and operations. For the majority of CHD and RHD patients, 2D echocardiographic diagnosis is sufficient for the majority of cases, whereas for CAD or structural disease and hemodynamic dysfunction, diagnostic cardiac catheterization is required.
At present there is no international umbrella like-structure or organization that coordinates or oversees the independent NGO volunteer activities, though some NGOs are developing more cooperative partnerships and projects. The USA NGOs (501C3 corporate USA foundations) are independent and rely on voluntary financial support and voluntary teams. The NGOs work as a donor partner with their host partner(s).
McQueen and colleagues (90) reported 99 humanitarian surgical organizations with a 46% response, and 17% with a cardiac program. Nguyen and colleagues (91) identified 80 NGOs worldwide supporting pediatric cardiovascular programs in 92 LMICS. At present, there are more than 40 active USA NGOs with CT surgical projects and programs abroad.
Turina (92) identified five different types of assistance: developmental assistance, donation of hospitals and equipment, NGOs, individual team visits to increase capacity, financial support of operations in developed centers, and education or training programs.
Dearani (93) suggests two types of host programs. The first is a twinning or partner center that involves a 5-10 year commitment. The second is a center that will never have an on-site program and will require a series of visiting teams. The Caribbean and Oceana islands are a unique situation in that there are many islands that are widespread with each island having a small population. This will require a system where patients can be transferred to a nearby hub for definitive care.
Dearani and colleagues (94) have also developed a practical strategic and tactical approach to the set-up and development of aspiring pediatric cardiac surgical programs.
The major CT surgery societies have developed a number of educational initiatives to address these challenges. They have also provided satellite conferences for NGOs at their annual meetings to increase awareness and interest. CTSNet has recently developed a volunteer portal to increase awareness (95). None of these organizations are actively involved with on-site host team developing projects or providing financial assistance.
There thus remains a need for dedicated and robust leadership to guide and coordinate the efforts of the independent NGOs, volunteer professionals, health care and industry donors, and the on-site host clinical centers. The major goals of the donor programs are to increase capacity and quality via team training and instilling experience and confidence in the host teams. The administrative, political, and logistical aspects must also be addressed. A memorandum of understanding of the donor and host programs must include benchmarks for completion and success. The rubrics should include awareness, access, accountability, sustainability, increasing capacity, transparency, quality control, and an exit strategy. There remains debate regarding the initial sequence of establishing pediatric cardiac surgery. Traditionally, adult thoracic surgery, then adult cardiac surgery, and finally pediatric cardiac surgery has been the sequence of development in LMICs and EEs. That has changed somewhat in that current activity focus primarily on pediatric cardiac surgery. There are several model examples of current NGO activities and efforts to reflect:
Collaborative and Cooperative Projects and Programs
- Fragiola and colleagues (96), in 2016, from Italy, highlight the organization of five groups working in cooperation, or synergy, on projects in Africa. The common goals are to provide knowledge and training support, along with financial assistance, infrastructure, equipment and supplies, and to support increased access to health care sources, primarily pediatric cardiac surgery.
- Bastero and colleagues (97), in 2017, reported a partnership model in four countries: Mexico, India, Vietnam, and Jamaica. They stressed the importance and value of teleconference, and the creation of hybrid programs that combine public and private hospital with NGOs to unify their efforts and resources.
Primary Solo Effort in One Country
- Liu (98) reviewed the model of the partnership between Boston Children’s Hospital and Project Hope with Shanghai Children’s Medical Center to develop the pediatric cardiac surgery program that now performs more than 4,000 pediatric open heart operations per year.
- Young and colleagues (99) reviewed a 25-year ongoing relationship in Russia. They developed an 8-step model in developing six congenital cardiac surgery programs.
Programs in Multiple Countries
- Chain of Hope is an example of NGOs working in multiple LMICs, especially in Africa and South East Asia, to build capacity in cardiac surgery (100).
- Molloy and colleagues (101), outlined the role of NGOs working in multiple countries and pointed out, in depth, tactical requirements necessary for successful individual team missions. The basic steps reflect the more than 30-year experience of Dr William Novick and his team working in many countries.
Regional Centers or Hubs
To improve the efficacy of all these approaches, there has emerged current interest and activity to establish regional hubs or centers of excellence both within countries and between countries. Calderon-Colmenero and colleagues (49), from Mexico, reported the recent example of establishing pediatric cardiac surgery centers in several areas of the country to allow more efficient access. Initially starting in single centers and then spreading into satellite centers is practical and cost effective.
Kinsley and colleagues (102) have established a CT surgery center and hub in South Africa that primarily serves the sub-Sahara region. This hub has partnered a private hospital with NGO support to provide adult and pediatric cardiac surgery support in the region. They have provided fellowship cardiac surgery training. These fellows then return to their native country to establish or supplement a cardiac surgery center, for example in Ghana (103).
Dr Devi Shetty, from Bangalore, India, has established a hub that combines clinical outreach with the domestic and international market. A unique cost-effective health insurance program has made access and affordability possible for the India LMIC population (104).
Embedding Concept
Recently, the concept of embedding has emerged. Dr Kathleen Fenton’s work in Nicaragua stresses the practical and cost saving value of long term continuity in a single host program (105). This is not a new concept, as voluntary missionary hospitals have been involved worldwide for many years (84). Embedding provides a micro approach to the needs and challenges of any given new or existing developing program, as opposed to the macro approached from short NGO missions.
Tefera and colleagues (106, 107), from Ethiopia, stress the need for cooperation of the foreign donor NGOs to provide a more organized sequential coverage scheme. This would begin with smaller teams, especially with individual visiting CT surgeons working closer with the local staff to accelerate the transfer of skills, knowledge, confidence, experience, and responsibility, thus accelerating the exit strategy.
Cox (108), in 2001, outlined a comprehensive strategic and tactical approach that addressed the challenges for CT surgery growth in LMICs and EEs, as well as the role of the major societies, corporations, and NGOs in that effort. This approach included the global education and training of CT surgery residents and fellows. The role and goal of volunteer groups would be to develop the best practices in delivering care in the different cultural and health care environments. The latter would be accomplished through both on-site and internet-based methodology. The world would be divided into regions and zones, with individual hubs and teams within the zones being responsible for developing and mentoring programs within their zones and regions (Table 4). A relook at this visionary approach is warranted. To extrapolate this further, over the past 17 years there has been a gradual shift of help and assistance from North America and Western Europe to the hubs and centers in the defined zones. This is especially true in Asia and the Pacific Rim. Examples include South Korea reaching out to Uzbekistan, Mongolia, and Vietnam. China is now involved in Vietnam, as well as Japan. Australia and New Zealand have been involved for many years as well in neighboring countries.
Health Resources
All countries have shortages, imbalance, and maldistribution of health resources. Worldwide there are 2,420 medical schools and 467 schools or departments of public health (109).There are about 59-100 million healthcare workers (doctors, nurses, midwives) with a need for 2.4 million more to provide the essential health care needs (110). There are 1 million new health care workers produced per year (doctors, nurses, midwives). The global expenditure for health care education is $100 billion, which is <2% of the global $5.5 trillion expenditure for global health care. The major shortfalls of an adequate health resource system include inadequate education and subsequent performance, job safety and security, job satisfaction, skill mix imbalance, increasing patient loads, stunted career advancement and development, continuing education, substandard work environment, no malpractice coverage, credentialing issues, and low salary and retirement programs. These concerns severely hinder recruitment and retention (111). The reasons for this include “curricular rigidities, professional silos, static pedagogy, insufficient adaptation to local contents, and commercialism in the professions” (110). This is accentuated by the lack of teamwork, cooperation, and leadership.
In addition, this situation is also worsened by the push/pull phenomenon, ie, factors pushing (diaspora or brain drain), and factors pulling workers away (recruitment incentives both within and without the country or region) (Figure 2). Quality education of health resources in LMICs is further compounded by disorganization and outdated teaching methods, along with inadequate funding at all levels (111).
In the USA, international medical graduates account for 25% of the clinical medical doctors. Of these, 25% are medical residents. All must have fulfilled the Educational Commission for Foreign Medical Graduates requirements (112-114). This is a major challenge given the increasing visa restrictions and requirements in the USA.
There is a shortage of CT surgeons in developed countries as well as in LMICs and EEs. In the USA, Grover and colleagues (115), in 2009, reported the average length of training time after medical school for CT surgery was 8.3 years. This has shortened now to a minimum of 6 years. In addition there were 4,734 active USA CT surgeons in 2005. There are now about 130 newly-trained CT surgeons per year. The supply will decrease by 18% in 2020. By 2025 there will be a shortage of 1,500 active CT surgeons or 25% of the projected need. Williams and colleagues (116), in 2010, projected a need of 5,169 CT surgeons by 2030. The active number then is projected at 3,000, leaving a need for at least 4,000 more. Filling the deficit will require additional well trained CT surgeons in the USA, as well as attracting qualified foreign-trained CT surgeons.
Women are a minority in CT surgery. Donington and colleagues (117) in 2012 noted that only 4.6% of USA CT Surgeons were women even though more than 40% of medical students were women. There has been a gradual increase of qualified and interested female candidates, but more are needed and wanted. A major effort has been seen with increased mentoring.
CT Surgery Education and Training Programs
In LMICs and EEs, as well as developed countries, the CT surgery residency challenges include attracting and selecting capable candidates, ie, with acceptable character, personality, and competence; increase in accredited education and training programs; shorter residency period; commitment to the specialty at a younger age; huge financial debt; “hands-on” experience; shorter work hours; early progressive responsibility, decision making, and problem solving; and suitable job placement and opportunities following successful completion of their residency and subsequent board certification.
At present, there is no universally accepted residency or fellowship model for CT surgery education, training, or certification. There are no global standards, requirements, or recommendations for graduate medical education (118).
Those countries with a program have their own system that may not be transportable or transparent in other countries. There are different pathways or combinations, ie, Ct, Tc, CV, CT. Exposure to critical care and general surgery, especially esophageal, vascular surgery, and chest trauma, varies in many international programs. Further advanced fellowships following residency are now desired or recommended for many job positions, especially, pediatric cardiac, transplantation and mechanical devices, minimally invasive approaches, robotic access, and transcatheter approaches.
Wood and Farjah (119), in 2009, assessed the global differences of CT surgery programs in a 38 item survey of 1,520 respondents. There were marked differences in the training programs and the major recommendation was greater cooperation between the global programs.
Replogle (118), in 2004, proposed an international CT surgery certification process. Yet it is difficult to develop international certification, requirements, or rules. However, there has been progress. The European Association for Cardio-Thoracic Surgery (EACTS) has developed a board of CT surgery that has enacted a syllabus and credentials examination that is a pathway to certification (120). However, this board does not have jurisdiction or oversight of the various residency programs. Loubani and colleagues (121) have advanced a European CT surgery residency model that is uniform and coherent. This would hopefully increase trust and transparency, as well as public confidence and acceptance.
In the USA, 12 years of primary education is followed by a four-year premedical undergraduate bachelor’s degree, then four years of medical school. Thereafter, each state or national board requires medical licensure. The graduate medical education CT surgery residency follows, which is now a minimum of five years of general surgery and two years of CT surgery training. This is followed by the successive completion of the two-part written and oral thoracic board examination. In many countries, only six years of medical university following primary school is required. Many USA residents are now seeking additional 1-2 years of specialty fellowship training. Finally, one must then be granted hospital privileges, completion of a proctoring period, and subsequent mandatory reboarding every 10 years thereafter (122, 123). Eventually, the integrated six-year program in the USA will displace the traditional programs and not require general surgery boards prior to the CT surgery residency program. Wood (123) has nicely reviewed the sequential changes in the USA system, along with the development of the two-pathway system, ie, the cardiac or thoracic pathway with separate index cases required.
Academic faculty recruitment and development needs to be increased and fostered. The roll of the faculty as coach, manager, instructor, and mentor needs to be better defined. Training the faculty requires the selection of qualified academic CT surgeons committed to the task of training the next generation in the newer technical procedures and operations, as well as supporting academic clinical and laboratory research and development. Academic activity in the developed programs has been challenged by the stress of increasing caseloads at the expense of decreased time for teaching and research.
Current residency and fellowship programs will require cooperation to establish rotations on specialties that include cardiology, vascular surgery, critical care, pulmonology, and oncology, depending on the CT dedicated pathway. This is in compliance with the increase in disease-specific specialties.
With regard to the global decrease in hands-on experience, attention has been given to supplement the training with corporate- or society-sponsored workshops. Reznick and MacRae (124) highlight the Fitts and Posner three-stage theory of motor skill acquisition: cognitive, integrative, and acquisition. Trehan and colleagues (125) have outlined a comprehensive overview of current systems in CT surgical areas. However, they have not been fully assessed or validated. There is still no substitute for the development of bedside care and operating room experience, along with the continuing development of judgment, confidence, maturity, and graded patient care responsibility. In the USA, the increase in high risk and technically more difficult cases has precluded ready opportunities for resident participation as the primary surgeon with supervised faculty surgeon support.
Historically, performance of a specific operation by the resident follows a traditional pattern and sequence: reviewing the operative choices and techniques, and discussing with the attending surgeon; then observing the operation; followed by being a second assistant, first assistant, primary surgeon with attending; and finally, primary surgeon with attending watching and commenting.
There is a need for international participation and support for the developing CT surgery residency programs regarding initiation, updating, and organization. Guidance and mentoring by mature and experienced academic clinical CT surgeons can be extremely helpful in this endeavor to help them grow, develop, and transfer their knowledge, judgment, and skills to the next generation. This would require at least six to 12 months of the embedding of experienced, academic foreign CT surgeons. As examples, model CT surgery residency programs have been initiated in both Shanghai, China (EE), and Ho Chi Minh City, Vietnam (LMIC), based on a modified USA model (126, 127).
These projects required strategic and tactical changes that were transferred in an organized and prospective manner. In China, recent changes in medical education have occurred (128). The Shanghai Health Bureau has now changed the medical resident status from hospital employee to resident, with salary support by the health bureau. In 2009, the Chinese Medical Doctor Association updated their medical education system. After five years of medical school, graduates would enter a three-year standardized residency programed before entering a specialization residency (128).
A major challenge in residency programs in the LMICs and EEs is a qualified and dedicated clinical faculty (training the trainers). Most of the staff have trained abroad in nonaccredited foreign programs, and are not adequately trained, willing, or able to participate in the education and training programs.
The developing programs should have a dedicated program director and administrative staff to coordinate and manage the residency and fellowship programs. This should include yearly in-service examinations, caseload logs, personal issues, overview of core conferences, clinical rotations, evaluation of the resident and staff, call schedule hours, attending CME meetings, job placement, further specialty training, simulation labs, salaries, personal health care and social needs, security/safety issues, and vacations.
Mentoring is extremely important and needed in recruiting interested candidates during medical school, through residency, and beyond into their clinical practice. Loop (129) nicely outlined the professional life into three phases: education, achievement, and payback. It is the latter phase where mentoring has its greatest role and satisfaction. Pasque (130) stresses the layout of the potential of the mentor and mentee, along with setting the goals for the education and training of future CT surgeons that include surgical excellence, teaching, research, and administrative participation in those areas that involve our specialty.
Mentoring should also persist beyond the residency period as the young CT surgeons frequently seek advice from their residency mentor(s) regarding medical and nonmedical topics and issues. As noted, active senior or retired CT surgeons are well suited to lead the charge to promote improvements and changes in the education and training of the next generation of CT surgeons in LMICs and EEs.
Loisance (131) gave a masterful insight into the training of young cardiac surgery residents in developing countries. He stressed the need for training in anesthesia and perfusion as well. Further, he points out that senior surgeons trained abroad are initially reluctant to teach the younger staff for a variety of reasons. Training requires a stepwise process that includes understanding, assimilation, and automation. Thereafter, the concentration is acquisition of the basic surgical protocols and procedures with senior surgery on-site supervision.
Recently there has been a trend for some CT surgery residents and junior staff to seek further hands-on experience, as well as exposure to different types of patients, in LMICs and EEs (132, 133). This endeavor benefits both the visiting residents and the host program.
Medical Tourism
Medical tourism includes “travel for the purpose of delivering care, or travel for the purpose of seeking health care” (134, 135). There are several scenarios:
- Self-paying or government-supported patients from LMICs, where service is not available or not of high quality, are pursuing care in developed centers abroad. This doesn't include nonpaying patients seeking free or low-cost care abroad.
- Self-paying patients from developed countries seeking care in other countries because of lower cost or because of limited insurance coverage or high co-payments.
- Private centers in EEs that cater to paying patients within their own country.
- Centers from developed countries establishing private for-profit hospitals in LMICs or EEs.
The advantages of private for-profit medical tourism include lower costs of drugs, devices (especially heart valves), wages, administrative costs, malpractice issues, decreased waiting times (eg, kidney transplants), and access to controversial procedures like stem cell therapy for heart failure. The major cardiac procedures performed are lower-cost CABG, heart valve replacement or repair, and PCI. The disadvantages include incomplete or lack of transparency regarding patient security, surgical results, quality of care, as well as follow-up arrangements and long-term results or concerns. Other issues are the process for determining the proper indications, evaluation, second opinions, and proper timing of surgery, as well as the risks, benefits, and complications related to the specific procedure(s) to be performed.
In 2008, the American College of Surgeons recommended that for patients seeking care at healthcare institutions abroad, those institutions meet the standards for accreditation as established by recognized accrediting organizations (136, 137). It is recognized that the standards are not universal and vary around the world.
A major challenge is determining whether these centers are safe and comply with established standards of care. Certification is helpful, but there is no established way to specifically establish patient safety (138). The USA-based Joint Commission International (JCI) established its international affiliate agency in 1999. More than 600 hospitals and clinical departments around the world now have JCI accreditation, and this is increasing by about 20% per year. The worldwide medical tourism market is growing at a rate of 15-25% annually. It is estimated that 1,400,000 Americans traveled abroad for medical care in 2016. The financial savings ranged from 20-90% (Brazil: 20-30%, Costa Rica: 45-65%, India: 65-90%, Malaysia: 65-80%, Mexico: 40-65%, Singapore: 25-40%, South Korea: 30-45%, Taiwan: 40-55%, Thailand: 50-75%, and Turkey: 50-65%) (138). Accreditation Canada International is another private nonprofit organization that is involved with increasing certification based on accepted standards of care (139).
The role of the major CT surgery societies in the certification or credentialing of these for-profit tourism centers has not been fully investigated or resolved. Jacobs and colleagues (140) debated the pros and cons of medical tourism with regards to certification. The Society of Thoracic Surgeons (STS) adult cardiac surgery database could be a model to develop, evaluate, and certify foreign centers. However, this would have to be a voluntary endeavor.
Health Information Technology
Information
Internet access, via computer or smart phone, is a major vehicle to transmit knowledge, skills, finance, techniques and information worldwide in real time. Health information technology (HIT) has changed the global landscape insofar as medical information, medical education, and patient consultation and care are concerned (141). The major functions of HIT are storing and processing data. There are several types of HIT at the clinical and administrative health care levels. They include the electronic health record, the personal health record, and the clinical data exchanges (142).
CTSNet has emerged as a major global site via the computer or smart phone for information, news, updates, blogs, and searches. Social media, health care websites, Google, and YouTube have complimented that effort.
Education
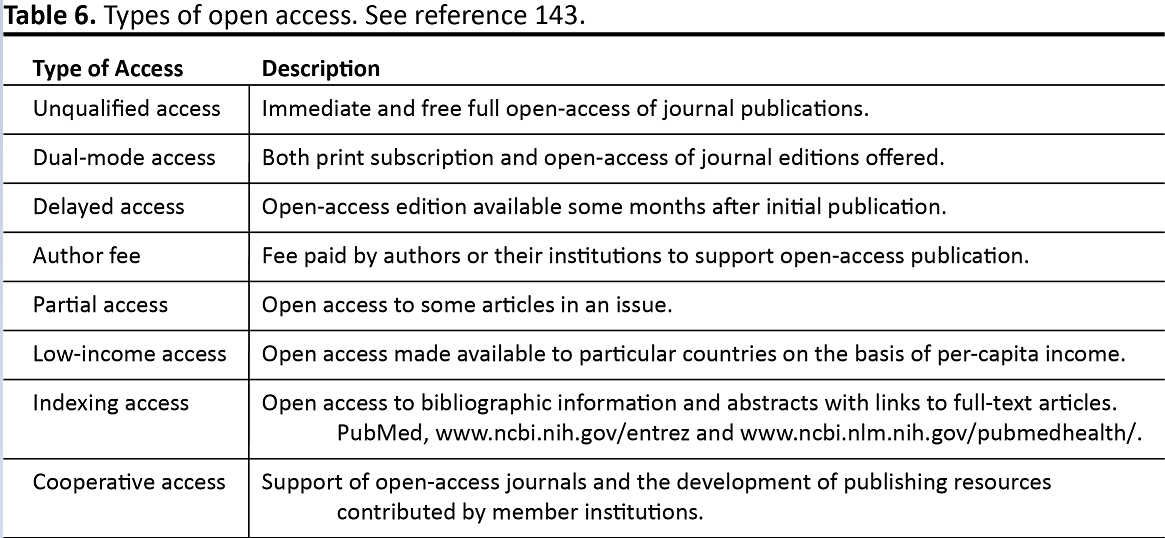
Online real-time conferences, meetings, lectures, symposia, workshops, daily rounds, and discussions supplement the on-site presence. With regards to hard copy, texts, monographs, manuals, journals, corporate information, personal notes, and other printed information can all be readily accessed and downloaded (143-145). Unfortunately, corporate protection and property ownership have been a stumbling block for full open access. Publishers own the copyrights to their journals and require payment to access their articles, as well as obtaining permission to publish any of the contents. Yet the individual institutions that purchase the journals, especially the medical schools, allow free access to those who qualify. Frank (143) proposed the access principle:
“A commitment to the value and quality of research carries with it a responsibility to extend the circulation of such work as far as possible and ideally to all who are interested in it and all who might profit by it.” (143)
Several types of open access approaches are summarized in Table 6.
Patient Care
Telemedicine incudes the transmission and management of health related information for patients, providers, payers, or other interested groups. The WHO defines telemedicine as:
“The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.” (146)
Medical technology continues to advance at a remarkable rate (142, 147, 148). Medical telecommunication is now available to transfer medical information, consultations, and individual patient data. Medical outsourcing of medical care, either as long-range patient management or diagnostic testing, is now readily available. Teleconsultation allows real-time interaction between experts in developed countries providing up to date assistance to developing countries. Related issues include cost, patient data privacy, consent and security, malpractice and liability, and compliance with local government laws, policies, and restrictions (149).
As noted in developed countries, electronic and personal health records are common, as are electronic hospital and clinic patient care documenting and monitoring. This has increased access and convenience, saves time and costs, and has increased quality and efficiency. This has virtually eliminated hard copy storage. However, this technology is not readily available in most LMICs and EEs.
In LMICs, telemedicine would be cost-effective, increase patient access to medical care, and decrease inaccurate or unavailable hard copy documentation and storage issues (141). Clinical screening of patients and follow-up care would also become a valuable and effective modality. This would decrease on-site travel to health care facilities, especially in rural areas, and poorly accessible urban enclaves.
Database, Guidelines, and Screening
At present there is no comprehensive international database or registry for CT surgery that includes the number of NGOs, cardiac centers, number of CT surgeons, allied health team members, annual caseloads, or surgical outcomes. It is estimated that 10,000 active CT surgeons in 6,000 centers globally perform more than 2 million open heart operations per year. This is based on poorly referenced data from the internet, CT surgery societies, the literature, corporate resources, and local personal contacts. STS and EACTS have developed clinical adult cardiac, pediatric cardiac, and thoracic surgery database systems, as well as guidelines for a variety of topics (150, 151). These areas could be potentially expanded globally to include annual number of cases performed, number of active surgeons, and operative results.
An accurate voluntary global audited database would certainly have value in projecting results and trends, as well as a vehicle for clinical and administrative research. Unfortunately, the cost, mixed interest, and politics of developing this project are difficult challenges.
A major present challenge is retrieving data from LMICs and EEs. A database is difficult to develop and maintain. The data may not be readily available or there may be reluctance to share their clinical data or results for a variety of reasons.
Shapira and colleagues (152) in 2014, from Israel, reported a collaborative study of several centers. They employed the STS model. This study stressed the ethical and transparency issues, as well as the need for leadership, determination, and financial support. Nguyen and colleagues (91), in 2014, performed a survey of 80 NGOs that supported CV programs in 92 LMICs. The ultimate goal was to establish a global database. Vener and colelagues (153), in 2017, cited over 30 worldwide CHD registries that included surgery, intensive care, cardiology, and anesthesia statistics.
Population screening in LMICs and EEs is effective for fetal surveillance as well as RHD detection. An example is RHD 2D echocardiographic screening in Mozambique (154). This has created a proactive approach to establish and monitor the management schemes. Developing a waiting list is helpful, but can be frustrating for patients and families, especially when the waiting list is long or the operation is postponed. Incorrect diagnosis, cost, contact methodology, and difficult or lost follow-up remain logistical challenges in LMICs and EEs.
An established database and screening program can yield important and valuable results. Jenkins and colleagues (155) reported the results of a collaborative database and registry project at 28 sites in 17 LMICs. The annual CHD surgery data benchmarking was analyzed. The key drivers of the study were safe perioperative practice, reduction of surgical site infection or sepsis, and team-based practice. This type of surveillance is a worthwhile model to maintain quality and oversight of outcomes.
Research and Development
Measure what is measurable, and make measurable what is not so.
~Galileo Galilei (156)
Research and development is the final phase of the development and growth of CT surgery in LMICs and EEs. There is a need for mentoring and guidance in the development of on-site clinical research and eventually laboratory research and translational applications. Clinical publications from LMICs and EEs have gradually increased in the high impact North American and European journals, especially from the non-English speaking countries. There is a continued need for English language grammar assistance and manuscript editing. For a number of years the author of this article has reviewed papers from China, Vietnam, Africa, Russia, and India. The goals were to correct the English grammar, and to edit those areas that are confusing, illogical, disorganized, or require more reference support.
As noted, access to free soft or hard copy references and paying for corporate permissions remains a major obstacle to an accurate and comprehensive review of the literature, as well as publishing papers. There is also increasing pressure in many LMICs and EEs CT surgery departments to submit papers primarily to high impact journals. A practical sequence approach is to start with case reports, clinical reviews, retrospective studies, and finally prospective studies.
Translational multinational collaboration studies are very helpful and important, since there is a greater patient pool from LMICs and EEs that can be balanced with expertise from academic centers and private research institutes in developed countries, as well as private corporations (157).
Other important issues include ethics and the quality of the submitted papers. International ethical standards and guidelines have been developed for clinical trials and therapeutic interventions (158, 159). Adherence to the ethical standards protects and supports the research rights of animal or human subjects, and it preserves public trust and confidence (160).
The quality of research papers, especially the randomized controlled trial (RCT), is crucial. Sade (161) has nicely outlined the Consolidated Standards of Reporting Trials (CONSORT), which was designed to increase the quality of RCTs. It comprises 22 items related to details of design and process, and a flow diagram of the progress through the trial.
The performance of both clinical and laboratory studies in partnership with LMICs and EEs, using local health resources, is beginning to grow. Examples of seminal work include Sir Magdi Yacoub’s work in Mozambique (162), KM Cherian in Chennai, India (163), and several cooperating Asian centers (164).
The funding of research is a worldwide challenge. The major financial sources include individual country public support, nonprofit foundations, private donations, and corporative support. In the USA, the federal government’s National Institute of Health is the largest research and development system in the world, with more than 300,000 researches in over 2,500 institutions, and an annual budget of more than 30 billion US dollars/year. Ten percent of that budget is allocated to the National Heart, Lung, and Blood Institute branch (165, 166).
Summary
I keep six honest serving-men, They taught me all I knew, Their names are What and Why and When, And How and Where and Who.
~Rudyard Kipling (167)
An understanding of the global background (S.P.E.E.D) is informative and necessary. The maldistribution of CT surgery between and within countries is slowly improving. Improved socioeconomic conditions in LMICs and EEs have witnessed major increases in CT surgical access and availability of procedures for the lingering prevalence of RHD and CHD, as well as the increase in CAD and degenerative diseases. As this clinical demand increases, the major challenges will remain increased access, cost control and support, availability of services, and qualified “in situ” health care personnel. The quality and quantity of CT surgery will require a continued increase in the number of CT surgeons and critical team members. The CT surgical societies, NGOs, and the international corporate sectors will need to continue playing an active role in that endeavor. As the volume and quality of surgery increase in LMICs and EEs, then a gradual weening of involvement will ensue and the maldistribution between and within countries will gradually dissipate.
References
- Quote. http://www.rebellesociety.com/2013/08/23/i-want-to-be-all-used-up-when-i-die-george-bernard-shaw-on-taking-creative-action/. Accessed January 11, 2018.
- Pezzella AT. Global aspects of cardiothoracic surgery with focus on developing countries. Asian Cardiovasc Thorac Surg Ann. 2010;18:299-310.
- Bygbjerg IC. Double Burden of Noncommunicable and Infectious Diseases in Developing Countries http://science.sciencemag.org/content/337/6101/1499.full Accessed January 22, 2018.
- Unger F. Worldwide survey on cardiac interventions 1995. CorEuropaeum. 1999;7:128-146.
- Intro to CPT coding http://www.medicalbillingandcoding.org/intro-to-cpt/ Accessed January 11, 2018.
- 2016 Selected Cardiothoracic Procedures Coding RESOURCE. http://www.medtronic.com/content/dam/medtronic-com-m/mdt/cardio/documents/cv_procedures_201602066aen.pdf Accessed January 11, 2018.
- Yankah C, Fynn-Thompson F, Antunes M, et al. Cardiac surgery capacity in Sub-Saharan Africa: quo vadis? Thorac Cardiovasc Surg. 2014;62:393-401.
- The Lancet: Surgery death rates in Africa are double the global average. https://www.eurekalert.org/pub_releases/2018-01/tl-tls010218.php Accessed January 21, 2018.
- Pocket World in Figures, 2017 edition. The Economist; 2016.
- The World Fact Book. https://www.cia.gov/library/publications/the-world-factbook/docs/profileguide.html Accessed January 11, 2018.
- Sociology definition. https://www.google.com/search?q=sociology+definition&rlz=1C1TSNP_enUS484US582&oq=sociology&aqs=chrome.1.69i57j0l5.6160j0j8&sourceid=chrome&ie=UTF-8efinition
- Huntington SP. The Clash of Civilizations and the Remaking of World Order. Penguin Books. London; 1996:45-48, 53-54.
- Marmot M. Health in an unequal world. Lancet. 2006;368:2081-2094.
- Syndemics. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(17)30003-X/fulltext Accessed January 11, 2018.
- Frenk J, Moon S. Governance challenges in global health. N Engl J Med. 2013;368:936-942.
- OECD. http://www.oecd.org/about/ Accessed January 23, 2018.
- Lex Mundi. http://www.lexmundi.com/lexmundi/International_Guide_on_Health_Industry_Laws.asp Accessed January 11, 2018.
- Medical Malpractice in Ecuador. https://cuencahighlife.com/doctors-protest-medical-malpractice-legislation/ Accessed January 11, 2018.
- Levitsky S. Navigating the new “flat world” of cardiovascular surgery. Ann Thorac Surg. 2007;83:361-369.
- World Bank. https://datahelpdesk.worldbank.org/knowledgebase/articles/378834-how-does-the-world-bank-classify-countries Accessed January 11, 2018.
- Leirner AA. The health and wealth of nations - coping with limited resources. Artificial Organs. 2006;30:493-497.
- Turina MI. Presidential address. European Association for Cardio-Thoracic Surgery: carrying the torch. Eur J Cardiothorac Surg. 2002;22:857-863.
- Environment issues. https://en.wikipedia.org/wiki/Geography and https://www.environmentalscience.org/ Accessed January 11, 2018.
- IPCC Climate Change 2014 - Synthesis Report. http://www.ipcc.ch/pdf/assessment-report/ar5/syr/SYR_AR5_FINAL_full_wcover.pdf Accessed January 11, 2018.
- McMichael AJ. Globalization, climate change and human health. N Engl J Med. 2013;368:1335-1349.
- Demographics. https://en.wikipedia.org/wiki/Demography Accessed January 11, 2018.
- Demographic Transition Model. https://www.google.com/search?q=demographic+transition&rlz=1C1TSNP_enS484US582&tbm=isch&tbo=u&source=univ&sa=X&ved=0ahUKEwi9jqrIjbTXAhWFPCYKHTHgDqUQiR4IzQE&biw=1366&bih=637#imgrc=D-MrVvomGErH2M Accessed January 11, 2018.
- Global population. https://en.wikipedia.org/wiki/World_population Accessed January 11, 2018.
- Malthusian Theory of Population http://cgge.aag.org/PopulationandNaturalResources1e/CF_PopNatRes_Jan10/CF_PopNatRes_Jan108.html Accessed January 11, 2018.
- Broadfoot M. Building a better harvest. Scientific American. 2017;317:67-73.
- West PC, Gerber JS, Engstrom PM, et al. Leverage points for improving global food security and the environment. Science. 2014;345:325-328.
- Food production. http://www.fao.org/docrep/014/mb060e/mb060e00.pdf Accessed January 11, 2018.
- You D, Anthony D, Wardlaw T, Jenkins R. The changing face of global child demographics. Lancer. 2013;381:701-703.
- What Is Globalization? http://www.globalization101.org/what-is-globalization/ Accessed January 11, 2018.
- Friedman TL. Thank You for Being Late. Picador Paperbacks. New York, NY; 2017:32-37.
- GBD 2015 mortality and cause of death collaborators. Global, regional, and national life expectancy, all cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burdon of Disease Study 2015. Lancet. 2016;388:1459-1544.
- Global Mortality. http://www.who.int/gho/mortality_burden_disease/en Accessed January 11, 2018.
- Norton R, Kobosingye O. Global health - injuries. N Engl J Med. 2013;368:1723-1730.
- GBD 2015 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1603-1658.
- GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1260-344.
- HDI. http://hdr.undp.org/en/content/human-development-index hdi Accessed January 11, 2018.
- GBD 2015 SDG Collaborators. Measuring the health-related Sustainable Development Goals in 188 countries: a baseline analysis from the Global Burden of Disease Study 2015. Lancet. 2016;388:1813-1850.
- Murray CLJ. Shifting to sustainable development goals - implications for global health. N Eng J Med. 2015;375:1390-1393.
- HDT Report 2016. http://hdr.undp.org/en/2016-report Accessed January 11, 2018.
- Joint WHO/World Bank new release. http://www.who.int/mediacentre/news/releases/2015/uhc-report/en/ Accessed January 23, 2018.
- Health Care Systems - Four Basic Models http://www.pnhp.org/single_payer_resources/health_care_systems_four_basic_models.php Accessed January 11, 2018.
- Mills A. Health care systems in low-and middle-income countries. N Engl J Med. 2014;370:552-557.
- Covey SR. The 3rd Alternative. Free Press. New York, NY; 2011:12-15.
- Calderon-Colmenero J, Cervantes-Salazar J, Curi-Curi P, Ramirez-Marroquin S. Congenital heart disease in Mexico: advances of the regionalization project. World J Pediatr Congenit Heart Surg. 2013;4:165-171.
- Pryor AD. Surgical Evaluation. Cooperation is the key. Arch Surg. 2005;140:237-240.
- Luckraza H, Norella MN, Buchb M, Jamesc R, Cooperd G. Structure and functioning of a multidisciplinary ‘heart team’ for patients with coronary artery disease: rationale and recommendations from a joint BCS/BCIS/SCTS working group. Eur J Cardiothorac Surg. 2015;48:524-529.
- Blumenfeld O, Na’amnih W, Shapira-Daniels A, Lotan C, Shohat T, Shapira OM. Trends in coronary revascularization and ischemic heart disease–related mortality in Israel. J Am Heart Assoc. 2017;6:e004734.
- Molina JAD, Heng BH. Global trends in cardiology and cardiothoracic surgery – an opportunity or a threat? Ann Acad Med Singapore. 2009;38:541-545.
- Gersh BJ, Sliwak K, Mayosi BM, Yusuf K. The epidemic of cardiovascular disease in the developing world: global implications. Eur Heart J. 2010;31:642-648.
- Roth GA, Forouzanfar MH, Moran AE, et al. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med. 2015;372:1333-1341.
- Coronary Artery Bypass Graft (CABG) Market Analysis. https://www.grandviewresearch.com/industry-analysis/coronary-artery-bypass-graft-cabg-market
- Gaziano TA. Economic burden and the cost-effectiveness of treatment of cardiovascular diseases in Africa. Heart. 2008;94:140-144.
- Boudoulas KD, Borer JS, Boudoulas H. Etiology of valvular heart disease in the 21st century. Cardiology. 2013;126:139-152.
- Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano. Burden of valvular heart diseases: a population based study. Lancet. 2006;308:1005-1011.
- Mvondo CM, Pugliese M, Giamberti A, et al. Surgery for rheumatic mitral valve disease in sub-saharan African countries: why valve repair is still the best surgical option. Pan African Medical Journal. 2016;2016:307. http://www.panafrican-med-journal.com/content/article/24/307/full Accessed January 11, 2018.
- Global Health. https://en.wikipedia.org/wiki/Global_health Accessed January 11, 2018.
- Franklin Delano Roosevelt. https://en.wikipedia.org/wiki/Right_to_health#Universal_Declaration_of_Human_Rights Accessed January 11, 2018.
- UN. www.fdrlibrary.marist.edu/archives/address_text.html Accessed January 11, 2018.
- Financing Global Health 2013. http://www.healthdata.org/sites/default/files/files/policy_report/2014/FGH2013/IHME_FGH2013_Full_Report.pdf Accessed January 11, 2018.
- Financing health care. https://ourworldindata.org/financing-healthcare/ Accessed January 11, 2018.
- Battat R, Seidman G, Chadi N, et al. Global health competencies and approaches in medical education: a literature review. BMC Medical Education. 2010;10:94.
- Peluso MJ, Forrestel AK, Hafler JP, Rohrbaugh RM. Structured global health programs in U.S. medical schools: a web-based review of certificates, tracks, concentrations. Acad Med. 2013;88:124-130.
- Ackerly DC, Udaya Kumar K, Taber R, Merson MH, Dzau YJ. Global medicine: opportunities and challenges for academic health science systems. Acad Med. 2011;86:1093-1099.
- McKinley D, Williams SR, Norcini JJ, Anderson MD. International exchange programs and U.S. Acad Med. 2008;832(10 suppl):S52-557.
- Duke NUS Medical School. https://www.duke-nus.edu.sg/ Accessed January 11, 2018.
- Johns Hopkins Medicine International. http://www.hopkinsmedicine.org/international/international_affiliations/index.html Accessed January 11, 2018.
- Cleveland Clinic Abu Dhabi, UAE. https://www.clevelandclinicabudhabi.ae/en/about-us/pages/default.aspx Accessed January 11, 2018.
- Meara JG, Leather AJM, Hagander LH, et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. https://www.surgeons.org/media/21830874/2015-04-26-RPT-Global-Surgery-2030_Lancet-Commission-Full-Report.pdf Accessed January 11, 2018.
- Ng-Kamstra JS, Greenberg SLM, Abdullah F, et al. Global surgery 2030: a roadmap for high income country actors. BMJ Global Health. 2016;1:e000011. http://gh.bmj.com/content/bmjgh/1/1/e000011.full.pdf Accessed January 11, 2018.
- Farmer PE, Kim JY. Surgery and global health: a view from beyond the OR. World J Surg. 2008;32:533-536.
- Duda RB, Hill AG. Surgery in developing countries. Bull Am Coll Surg. 2007;92:12-18.
- Meara JG, Hagander L, Leather AJM. Surgery and global health: a Lancet commission. Lancet. 2014;383:12-13.
- Greenberg SLM, Vega MP, Bowder AN, Meara JG. The Lancet Commission on Global Surgery makes progress in first year of work. Bull Am Coll Surg. 2015;100:23-28.
- Raykar N, Mukhopaghya S, Ng-Kamstra JS, et al. Progress in achieving universal access to surgical care: an update and a path forward. Bull Am Coll Surg. 2016;101:12-18.
- Weiser TG, Regenbogen SE, Thompson KD, et al. An estimation of the global volume of surgery: a modelling strategy on available data. Lancet. 2008;372:139-144.
- Rose J, Weiser TG, Hider P, Wilson L, Gruen RL, Bickler S. Estimated need for surgery worldwide based on the prevalence of diseases: a modeling strategy for the WHO global health estimate. Lancet Global Health. 2015;3(s2):S13-S20.
- Shrime MG, Dare AJ, Alkire BC, O’Neill K, Meara JG. Catastrophic expenditure to pay for surgery worldwide: a modelling study. Lancet Glob Health. 2015;3(S2):S38-S44.
- Bickler SW, Spiegel D. Improving surgical care in low- and middle-income countries: a pivotal role for the World Health Organization. World J Surg. 2010;34:386-390.
- Ozgediz D, Hsia R, Weiser T, et al. Population health metrics for surgery: effective coverage of surgical services in low-income and middle-income countries. World J Surg. 2009;33:1-5.
- Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Eng J Med. 2009;360:491-49.
- WHO Surgery Manual. http://www.who.int/surgery/publications/en/SCDH.pdf Accessed January 11, 2018.
- Pezzella AT. Volunteerism and humanitarian efforts in surgery. Curr Prob Surg. 2006;43:837-932.
- Nguyen N, Pezzella AT. Pediatric cardiac surgery in low-middle-income countries or emerging economies: a continuing challenge. World J Ped Cong Heart Surg. 2015;6:274-283.
- Musa NL, Hjordal V, Zheleva B, et al. The burden of paediatric heart disease. Cardiol Young. 2017;27(Suppl6):S3-S8.
- McQueen KAK, Hyder JA, Taira BR, Semer N, Burkle Jr FM, Casey KM. The provision of surgical care by international organizations in developing countries: a preliminary report. World J Surg. 2010;34:397-402.
- Nguyen N, Jacobs JP, Dearani JA, et al. Survey of nongovernmental organizations providing pediatric cardiovascular care in low- and middle-income countries. World J Ped Cong Heart Surgery. 2014;5:248-255.
- Turina M. Transfer of surgical knowledge: a continuous challenge. S A Heart. 2011;8:130-131.
- Dearani JA. Charitable outreach in cardiothoracic surgery: ingredients for success. World J Ped Card Heart Surg. 2016;7:732-733.
- Dearani JA, Jacobs JP, Bolman M, et al. Humanitarian outreach in cardiothoracic surgery: from setup to sustainability. Ann Thorac Surg. 2016;102:1004-1011.
- CTSNet. https://www.ctsnet.org/surgical-volunteerism Accessed January 11, 2018.
- Frigiola A, Moussaidi N, Giamberti A, et al. International cooperation in healthcare: model of IRCCS Policlinico San Donato and Bambini Cardiopatici nel Mondo Association for congenital heart diseases. Eur Heart J. 2016;18(SupplE):E72-E78.
- Bastero P, Staveski SL, Zheleva B, et al. Parent education discharge instruction program for care of children at home after cardiac surgery in Southern India. Cardiol Young. 2017;27(Suppl6):S55-S60.
- Liu J. Challenges and progress of the pediatric cardiac surgery in Shanghai Children's Medical Center: a 25-year solid collaboration with Project HOPE. Sem Thorac Cardiovasc Surg. 2009;2:12-18.
- Young JN, Everett J, Simsic JM, et al. A stepwise model for delivering medical humanitarian aid requiring complex intervention. J Thorac Cardiovasc Surg. 2014;148:2480-2489.
- Chain of Hope. https://www.chainofhope.org/ Accessed January 11, 2018.
- Molloy FJ, Nguyen N, Mize M, et al. Medical missions for the provision of paediatric cardiac surgery in low- and middle-income countries. Cardiol Young. 2017;(Suppl6):S47-54.
- Kinsley RH, Edwin F, Colsen PR, Mamorare H, Martin G, Brink J. Paediatric cardiac surgery for a continent - the experience of the Walter Sisulu Paediatric Cardiac Centre for Africa. SA Heart. 2011;8:122-129.
- Edwin F, Tettey M, Aniteye E, et al. The development of cardiac surgery in West Africa - the case of Ghana. Pan African Medical J. http://www.panafrican-med-journal.com/content/article 9/15/full/
- Narayana Health. https://www.narayanahealth.org/
- Fenton K. A Global Practice: My experience with cardiothoracic surgery mission work. https://www.ctsnet.org/article/global-practice-my-experience-cardiothoracic-surgery-mission-work
- Tefera E, Nega B, Yadeta D, ChanieY. Humanitarian cardiology and cardiac surgery in sub-Saharan Africa: can we reshape the model? World J Ped Heart Surg. 2016;7:727-731.
- Tefera E. Treatment of children with rheumatic heart disease in Sub-Saharan Africa by overseas’ medical missions: challenges left behind. J Cardiol Clin Res. 2014;2:2-6.
- Cox JL. Presidential address: changing boundaries. J Thorac Cardiovasc Surg. 2001;122:413-418.
- Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376:1923-1958.
- Kuehn BM. Global shortage of health workers, brain drain stress developing countries. JAMA. 2007;298:1853-1855.
- Crisp N, Chen L. Global supply of health professionals. N Engl J Med. 2014;370:950-957.
- McMahon GT. Coming to America - international medical graduates in the United States. N Engl J Med. 2004;350:2435-2437.
- Education Commission for Foreign Medical Graduates (ECFMG). http://www.ecfmg.org/certification/index.html Accessed January 11, 2018.
- Eckhert NL, van Zanten M. U.S.-citizen international medical graduates - a boon for the workforce. N Engl J Med. 2015;372:1686-1687.
- Grover A, Gorman K, Dall TM, et al. Shortage of cardiothoracic surgeons is likely by 2020. Circulation. 2009;120:488-494.
- Williams TE, Sun B, Ross P, Thomas AM. A formidable task: population analysis predicts a deficit of 2,000 cardiothoracic surgeons by 2030. J Thorac Cardiovasc Surg. 2010;139:835-840.
- Donington JS, Litle VR, Sesti J, Colson YL. The WTS report on the current status of women in cardiothoracic surgery. Ann Thorac Surg. 2012;94:452-459.
- Replogle RL. A proposal for international certification in cardiothoracic surgery. Asian Cardiovasc Thorac Ann. 2004;12:187-188.
- Wood D, Farjah F. Global differences in the training, practice, and interrelationship of cardiac and thoracic surgeons. Ann Thorac Surg. 2013;95:201-206.
- EACTS. http://www.eacts.org/educational-events/ebcts/ Accessed January 11, 2018.
- Loubani M, Sadaba JR, Myers PO, et al. A European training system in cardiothoracic surgery: is it time? Eur J CardioThorac Surg. 2013;43:352-357.
- Ward ST, Smith D, Andrei AC, et al. Comparison of cardiothoracic training curricula: integrated six-year versus traditional programs. Ann Thorac Surg. 2013;95:2051-2056.
- Wood DE. The future of cardiothoracic surgery: a view from North America. Eur J Cardiothorac Surg. 2013;43:241-243.
- Reznick RK, MacRae H. Teaching surgical skills - changes in the wind. N Engl J Med. 2006;355:2664-2695.
- Trehan K, Kemp CD, Yang SC. Simulation in cardiothoracic surgical training: where do we stand? J Thorac Cardiovasc Surg. 2014;147:18-24.
- Pezzella AT. Initiation of a model six year cardiothoracic surgery residency program in Shanghai, China. Afr Ann Thorac Cardiovasc Surg. 2009;4:81-99.
- Pezzella AT. Model 5 year cardiothoracic surgery residency program in Ho Chi Minh City, Vietnam. Afr Ann Thorac Cardiovasc Surg. 2014;9:7-16.
- China. http://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(17)31921-9.pdf Accessed January 11, 2018.
- Loop F. Mentoring. J Thorac Cardiovasc Surg. 2000;119:S45-S48.
- Pasque M. Extreme mentoring in cardiothoracic surgery. J Thorac Cardiovasc Surg. 2015;150:785-789.
- Loisance DY. Training young cardiac surgeons in developing countries. Asian Cardiovasc Thorac Ann. 2012;20:384-386.
- Henry JA, Groen RS, Price RR, et al. The benefits of international rotations to resource-limited settings for U.S. surgery residents. Surgery. 2013;153:445-454.
- Humanitarian Cardiac Surgery: A Trainee’s Perspective. https://www.ctsnet.org/article/humanitarian-cardiac-surgery-trainee%E2%80%99s-perspective Accessed January 11, 2018.
- Reed CM. Medical tourism. Med Clin N Am. 2008;92:1433-1446.
- Patients Beyond Borders. https://www.patientsbeyondborders.com/medical-tourism-statistics-facts Accessed January 11, 2018.
- Unti JA. Medical and surgical tourism. Bull Am Col Surg. 2009;94;4:18-25.
- ACS Medical Tourism. https://www.facs.org/about-acs/statements/65-surgical-tourism Accessed January 11, 2018.
- Joint Commission International (JCI). https://www.jointcommissioninternational.org/achieve-accreditation/ Accessed January 11, 2018.
- Accreditation Canada International. http://www.iqg.com.br/docs/01302885656.pdf Accessed January 11, 2018.
- Jacobs JP, Horowitz MD, Mavroudis C, Siegel A, Sade RM. Surgical tourism: the role of cardiothoracic surgery societies in evaluating international surgery centers. Ann Thorac Surg. 2013;96:8-14.
- Role of Telemedicine in Developed and Under-Developed Countries. https://internetinitiative.ieee.org/newsletter/may-2017/role-of-telemedicine-in-developed-and-under-developed-countries Accessed January 11, 2018.
- Blumenthal D, Glaser JP. Information technology comes to medicine. N Engl J Med. 2007;356:2527-2534.
- Frank M. Access to the scientific literature - a difficult balance. N Engl J Med. 2006;354:1552-1555.
- Liesegang TJ, Schachat AP, Albert DM. The open access initiative in scientific and biomedical publishing: fourth in the series in editorship. Am J Ophthol. 2005;139:156-167.
- Open Access. https://www.plos.org/open-access Accessed January 11, 2018.
- TELEMEDICINE in Member States. Opportunities and developments. Report on the second global survey on eHealth Global Observatory for eHealth series – Volume 2. http://www.who.int/goe/publications/goe_telemedicine_2010.pdf Accessed January 11, 2018.
- Singh SN, Wachter RM. Perspectives on medical outsourcing and telemedicine - rough edges in a flat world. N Engl J Med. 2008;358:1622-1627.
- Dorsey ER, Topol EJ. State of telehealth. N Engl J Med. 2016;375:154-161.
- Summary of the HIPAA Security Rule. https://www.hhs.gov/hipaa/for-professionals/security/laws-regulations/index.html Accessed January 11, 2018.
- STS database. https://www.sts.org/registries-research-center/sts-national-database Accessed January 11, 2018.
- EACTS database. https://academic.oup.com/ejcts/article/44/3/e175/635878 Accessed January 11, 2018.
- Shapira OM, Badhwar V, Shahian D, et al. International participation in the Society of Thoracic Surgeons national database. Ann Thorac Surg. 2014;97:1127-1113.
- Vener DF, Gaies M, Jacobs JP, Pasquaili SK. Clinical databases in congenital and pediatric cardiac surgery, cardiology, critical care, and anesthesiology worldwide. World J Ped Cong Heart Surgery. 2017;8:77-87.
- Marijon E, Celemajer DS, Tafflet M, et al. Rheumatic heart disease screening by echocardiography. Circulation. 2009;120:663-668.
- Jenkins KJ, Castaneda AR, Cherian KM, et al. Reducing mortality and infections after congenital heart surgery in the developing world. Pediatrics. 2014;134:e1422-e1430.
- Galilio. https://www.brainyquote.com/quotes/galileo_galilei_381325 Accessed January 11, 2018.
- Translational research. https://en.wikipedia.org/wiki/Translational_research Accessed January 21, 2018.
- Kolman JM, Wray NP, Ashton CM, Wenner DM, Jarman AF, Brod BA. Conflicts among multinational ethical and scientific standards for clinical trials of therapeutic interventions. J Law Med Ethics. 2012;40:99-121.
- International Ethical Guidelines for Health-Related Research Involving Humans. https://cioms.ch/wp-content/uploads/2017/01/WEB-CIOMS-EthicalGuidelines.pdf Accessed January 11, 2018.
- Block MI, Khitin LM, Sade RM. Ethical process in human research published in thoracic surgery journals. Ann Thorac Surg. 2006;82:6-12.
- Sade RM. “Surgical research or comic opera” Redux. Ann Thorac Surg. 2006;82:1173-1174.
- Mocumbi AO, Ferreira MB, Sidi D, Yacoub MH. A Population study of endomyocardial fibrosis in a rural area of Mozambique. N Engl J Med. 2008;359:43-49.
- Frontier Mediville. http://frontiermediville.com/ResearchAndDevelopment.html Accessed January 11, 2018.
- Fatt JK, Tay E. Transcatheter aortic valve implantation in Asia. Ann Cardiothorac Surg. 2017;6:504-509.
- National Institutes of Health. https://www.nih.gov/about-nih/what-we-do/budget Accessed January 11, 2018.
- National Institutes of Health. https://www.nhlbi.nih.gov/about Accessed January 11, 2018.
- Rudyard Kipling. http://members.optusnet.com.au/charles57/Creative/Techniques/elephants_child.htm- Accessed January 11, 2018.
Appendix 1.
NGOs primarily focused on pediatric cardiac surgery.
Bambini Cardiopatici nel mondo: www.bambinicardiopatici.it
Caribbean Heart Mender: www.caribbeanheartmenders.org/
Cardiostart: www.cardiostart.com
La Chaine de L'Espoir (Chain of Hope): www.chainedelespoir.org/sites/uk/
Chain of Hope: www.chainofhope.org
Children's HeartLink: www.childrensheartlink.org
East Meets West: www.eastmeetswest.org
Foundation Mauritanienne du Coeur: www.mauritanie-coeur.org
Frontier Lifeline, India: www.frontierlifeline.com
Gift of Life International, Inc: www.giftoflifeinternational.org/
Global Healing: www.globalhealing.org
Global Heart Network: www.globalheartnetwork.net/
Global Impact: www.charity.org/index.html
Haitian Hearts: www.haitianhearts.org
Healing the Children: www.healingchildren.org
Hearts Around the World: www.hearts-aroundtheworld.org
Heartbeat International Foundation: www.heartbeatsaveslives.com
Heart Care International: www.heartcareintl.org
Heart to Heart International Children's Medical Alliance: www.heart-2-heart.org/
Hearts for All: www.coeurspourtous.ch/
International Children's Heart Foundation: www.ichf.org.www.babyheart.org/
International Children's Heart Fund: www.ichfund.org
International Hospital for Children: www.healachild.org
Novick Cardiac Alliance: www.cardiac-alliance.org
Open Heart International: www.ohi.org.au
Palestine Children's Relief Fund: www.pcrf.net
Pan-African Academy of Christian Surgeons: www.paacs.net
Partners in Health: www.pih.org
Project Haiti Heart: www.projecthaitiheart.org
Project Hope: www.projecthope.org
Project Open Hearts: www.poh.org
Project Medishare: www.projectmedishare.org
Russian Gift of Life, USA: www.rgol.org
Samaritan's Purse-International Relief: www.samaritanspurse.org
Satellife-Procor: www.procor.org
Save A Childs Heart: www.saveachildsheart.com
Surgeons of Hope Foundation: www.surgeonsofhope.org
Team Heart – Rwanda: www.teamheart.org/
The Heart of a Child Foundation; Little Hearts on the Mend: www.heartofachild.org
Variety - The Children’s Lifeline: www.varietychildrenslifeline.org/
Vina Capital Foundation: www.vinacapitalfoundation.org
Walter Sisulu Paediatric Cardiac Foundation: www.wspcca.org.za
World Pediatric Project: www.worldpediatricproject.org