ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Management of a Complex Aortic Dissection with Combined Open and Endovascular Techniques
Index
INDEX
Acute Type A aortic dissections can be challenging entities for cardiac surgeons and require close follow-up secondary to their propensity for aneurismal degeneration. A combined open and endovascular technique is described for treating the inital dissection and resultant complications.

Introduction
A Stanford type A aortic dissection is a life-threatening condition usually requiring emergent surgery. The mortality after repair has been reported as high as 30%1 although most recent series demonstrate mortality in the 10-16% range2,3 after surgical repair. Without intervention, early death occurs in 30% by 24 hours, 50% by 48 hours and 93% at 1 year as a result of malperfusion syndromes, cardiac complications or rupture4. Operative survivors also have high a high incidence of re-operation; 5% at 1 year, 10% at 5 years and 25% at 10 years5. Re-operation is typically required for aneurysmal dilatation of the residual dissection.
This case report details the aggressive potential for progression requiring multiple interventions in just the first year of follow-up of a type A aortic dissection. This patient has no family or personal history of a connective tissue disorder, bicuspid valve or other more rare risk factors for aggressive disease. This demonstrates that all dissections require not only close follow up but also early intervention.
Case Presentation
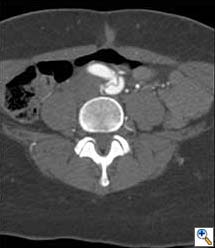
A 49-year-old woman with a history of hypertension and smoking presented to an outside hospital with sudden onset chest pain and hypotension. Computed Tomography/ Angiography (CTA) of the chest and abdomen revealed a type A aortic dissection extending from the ascending aorta to the left common iliac artery. (Figure 1) Of note, there was a significant pericardial effusion and left pleural effusion. Due to her hypotension and tamponade physiology, the patient was rapidly intubated followed by unsuccessful pericardiocentesis. The patient was then transferred to our institution for emergent dissection repair.
Figure 1a-e. Computed Tomography/Angiography (CTA) at
presentation demonstrating a type A aortic dissection.
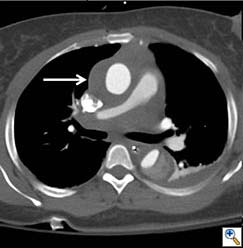
Figure 1a. Axial CT at level of the pulmonary artery. The false lumen in the ascending aorta (white arrow) has minimal flow.

Figure 1b.
Figures 1b-d. Axial CT cuts demonstrating the dissection continuing into the left common iliac artery.
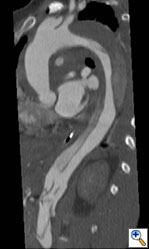
Figure 1e. Oblique sagittal CT reconstruction demonstrates the Type A dissection is complex with multiple fenestrations in the abdomen. Note bovine arch anatomy.
She was followed closely and a CTA was repeated at 3 months. This revealed minimal changes to the repaired aorta. However, at 6 months the follow-up CTA demonstrated an abrupt dilation of the descending aorta from 3.9cm to 6.5cm. (Figure 3) After extensive discussion, the patient returned to the operating room for a descending aortic replacement. Due to involvement of the distal arch, hypothermic circulatory arrest was utilized with an open proximal anastomosis just distal to the left subclavian artery origin down to T8 with a 26mm Gelweave graft (Vascutek Ltd). A lumbar drain was placed for spinal cord protection due to the distal extent of the repair. The false lumen pressurized at reperfusion, but would likely thrombose over time and was left alone. The patient recovered quickly and was discharged home on hospital day eleven with excellent impulse control.
The patient underwent repeat CTA 1 month later which demonstrated thrombosis of the false lumen except for a 4.5 x 4.6cm pseudoaneurysm proximal to the distal repair. (Figure 4) Since the new finding appeared to have a defined neck, the possibility of an endovascular exclusion of the fenestration was discussed with the back-up plan being either open or hybrid arch replacement. The patient underwent a carotid subclavian bypass using an 8mm Gore-Tex ring graft (WL Gore & Associates Inc, Flagstaff, AR) to extend the proximal landing zone. Aortic coverage was planned from the combined origin of the brachiocephalic and left common carotid arteries (bovine arch anatomy) down into the previously placed tube graft. Two days later, two Cook TX2 thoracic endografts (Cook Inc, Bloomington, IN) 30 x 120mm and 36 x 127mm were overlapped to exclude the intimal defect. Completion angiography demonstrated contrast in the proximal subclavian without perfusion of the false lumen. (Figure 5)
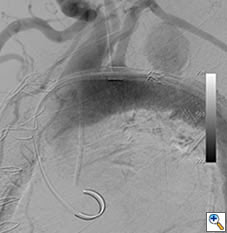
Figure 5a. Intraoperative angiogram demonstrating 4.4 x 4.6cm pseudoaneurysm distal to the left subclavian artery.
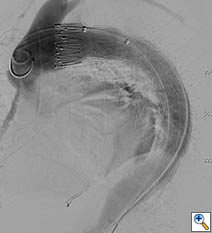
Figure 5b. Angiography after carotid-subclavian bypass and exclusion of pseudoaneurysm with a Cook TX2 thoracic graft. Note bovine arch anatomy with combined origin of brachiocephalic and carotid arteries.
Conclusion
Utilizing an aggressive follow-up regimen, this patient has survived 3 serious complications of her Type A dissection over the course of a year. Employing a combination of open and endovascular approaches, these complications have been dealt with safely and effectively. This highlights the increasing reliance on a multi-disciplinary approach to complex aortic disease. Additionally, these patients require close follow-up and imaging even in the absence of significant predictors for aggressive disease.
References
- Mehta RH, Suzuki T, Hagan PG; International Registry of Acute Aortic Dissection (IRAD) Investigators. Predicting death in patients with acute type a aortic dissection. Circulation. 2002 Jan 15;105(2):200-6.
- Goda M, Imoto K, Suzuki S, Uchida K, Yanagi H, Yasuda S, Masuda M. Risk analysis for hospital mortality in patients with acute type a aortic dissection. Ann Thorac Surg. 2010 Oct;90(4):1246-50.
- Moon MR. Approach to the treatment of aortic dissection. Surg Clin North Am. 2009 Aug;89(4):869-93.
- Hirst Jr AE, Johns Jr V, Kime Jr SW. Dissecting aneurysm of the aorta: a review of 505 cases. Medicine (Baltimore). 1958 Sep;37(3):217-79.
- Zierer A, Voeller RK, Hill KE, Kouchoukos NT, Damiano RJ Jr, Moon MR. Aortic enlargement and late reoperation after repair of acute type A aortic dissection. Ann Thorac Surg. 2007 Aug;84(2):479-86; discussion 486-7.