ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
A Rare Case of Paraganglioma Presenting as Anginal Pain
Kumar, Palli Venkata Naresh (2017): A Rare Case of Paraganglioma Presenting as Anginal Pain.
CTSNet, Inc.. https://doi.org/10.25373/ctsnet.5134795
Retrieved: 19:26, Jun 26, 2017 (GMT)
Case Report
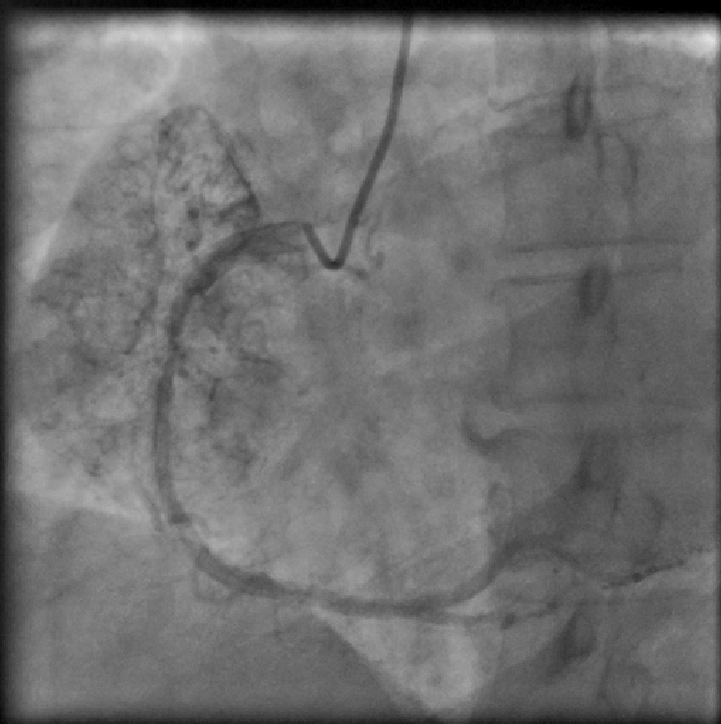
A 39-year-old female patient presented with complaints of retrosternal chest pain and shortness of breath associated with giddiness for the five days preceding the visit. She also complained of weight loss over the past two months. Six months prior, she underwent a coronary angiogram for similar complaints, which revealed normal epicardial coronary arteries with no atherosclerosis and an arteriovenous (AV) fistula in the right coronary artery (RCA). The patient had a history of hypertension and of pulmonary tuberculosis, which was treated medically.
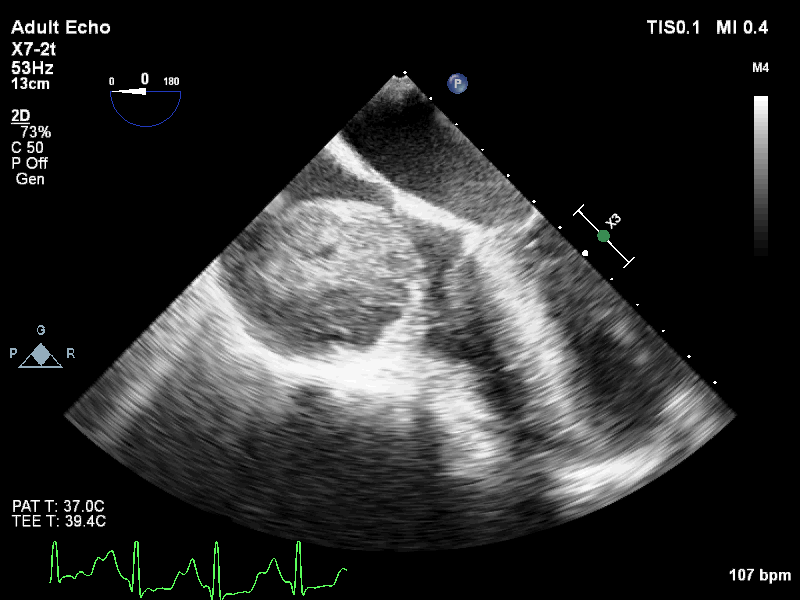
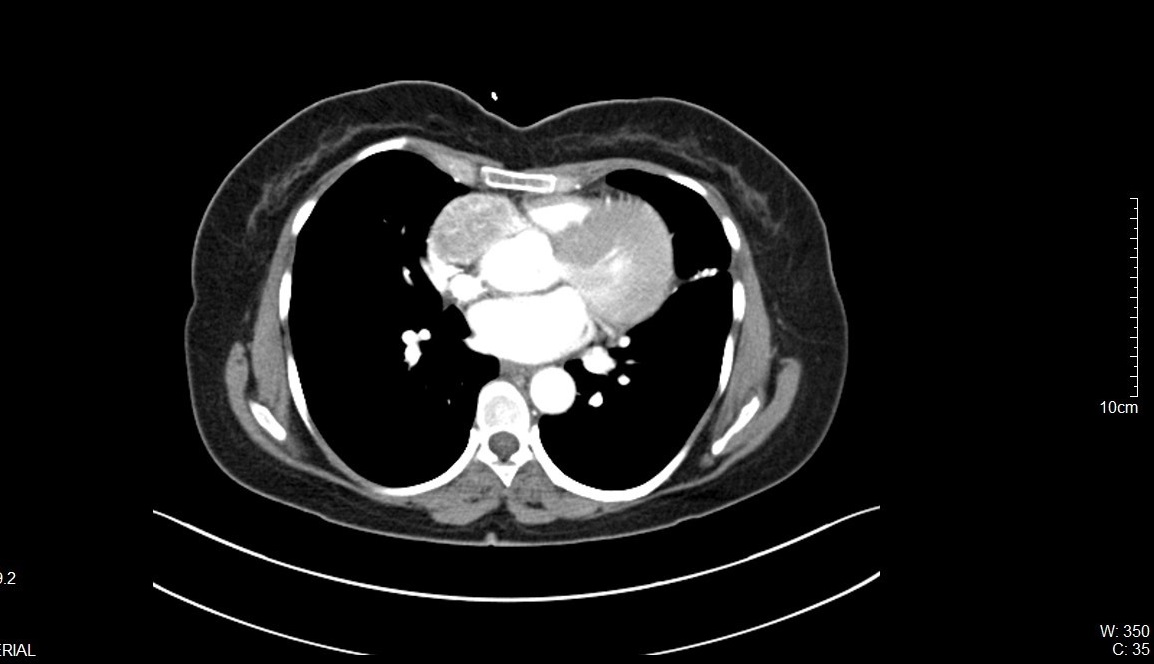
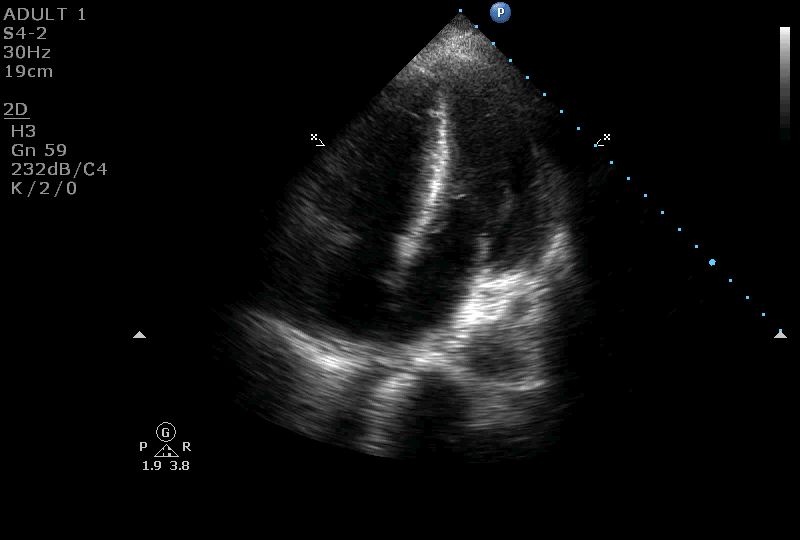
On further evaluation, the patient’s echocardiogram showed a 4.5 x 4.3 cm cystic tumor in the right atrium, hypertrophied obstructive cardiomyopathy with moderate left ventricular outflow tract obstruction, and good left ventricular function. She also underwent computed tomography (CT) and magnetic resonance imaging (MRI) of the chest, which revealed a neoplastic mass lesion, most likely right atrial myxoma.
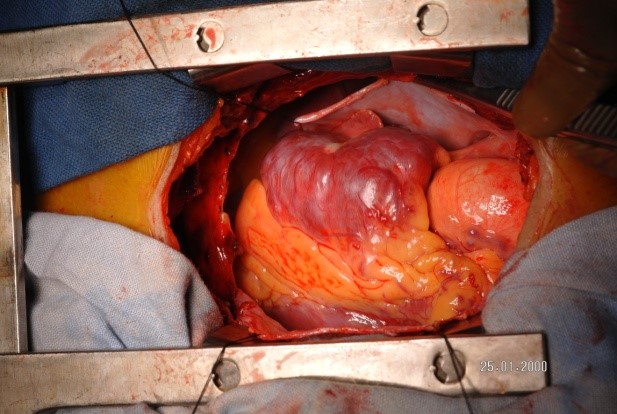
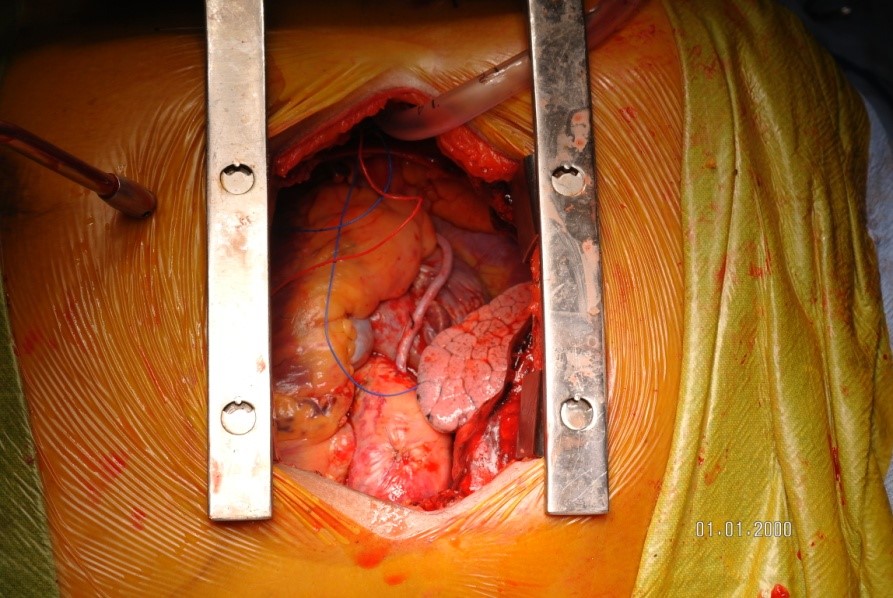
The patient was taken to surgery for a right atrial myxoma excision. A median sternotomy and pericardiotomy was done. Surprisingly, upon examination an 8 x 5 cm mass was found outside the right atrium (RA), adherent to part of the RA wall and encircling the RCA. The patient was placed on cardiopulmonary bypass with cardioplegic arrest. The mass was carefully dissected and removed en-bloc along with part of the RCA. The ostium of the RCA was sutured and buried. Pericardium was harvested and used to reconstruct the RA wall. The tricuspid valve was examined and checked for valve regurgitation. A saphenous vein graft was harvested from the left leg. The distal anastomosis to the RCA and the proximal anastomosis to the aorta were done with 7-0 and 6-0 prolene sutures, respectively. Distal flow was confirmed with a Doppler probe. The patient was gradually weaned off of cardiopulmonary bypass and the chest was closed in layers.
The excised mass was sent for histopathological examination where a gross cut section showed a yellowish to greyish-brown mass. Microscopic examination revealed nests of oval to elongated cells with eosinophilic cytoplasm, oval to elongated nuclei, and fine chromatin, morphology that is consistent with paraganglioma. An immunohistochemistry panel showed tumor cells positive for chromogranin A and synaptophysin, confirming the paraganglioma diagnosis.
Discussion
A large number of neoplasms and cysts exist in the mediastinum. Neurogenic tumors are the most common, accounting for approximately 20% of all mediastinal neoplasms. Usually located in the posterior mediastinum, neurogenic tumors originate from: (i) sympathetic ganglia (ganglioma, ganglioneuroblastoma, and neuroblastoma); (ii) intercostal nerves (neurofibroma, neurilemmona, and neurosarcoma); (iii) paraganglion cells (paraganglioma).
Mediastinal paragangliomas are rare, representing 1% of all mediastinal tumors and <2% of all pheochromocytomas. Patients present with symptoms of excess catecholamine production, including periodic/sustained hypertension, orthostatic hypotension, hypermetabolic state manifested by weight loss, hyperhidrosis, palpitations, headaches, and unusually with anginal pain.
Mediastinal paragangliomas are diagnosed by measuring urinary catecholamines and their metabolites, metanephrines and vanillylmandelic acid. Tumor localization is done with the help of CT, I-MIBG scintigraphy, and MRI. Because of the high vascularity of these lesions, contrast medium administration enhances CT.
Treatment of mediastinal paragangliomas includes surgical resection. Preoperative alpha adrenergic blockers and beta blockers are necessary to prevent hypertension and arrhythmias during tumor manipulation. Metastasis occurs in around 3% of patients. Alpha methyl tyramine (tyrosine hydroxylase inhibitor), which blocks the catecholamine synthesis, helps in controlling symptoms. About 10% of patients have multiple paragangliomas, and this is more common in patients with multiple endocrine neoplasia, familial history, or Carney syndrome.
References:
- Mohammad Tahir, MBBS, Syed Javad Noor, MBBS, Aravind Herle, MD, and Stephen Downing, MD. Right Atrial Paraganglioma A Rare Primary Cardiac Neoplasm as a Cause of Chest Pain. Tex Heart Inst J. 2009; 36(6): 594–597
- Tabindeh J Khalid, Omer Zuberi, Lara Zuberi,and Imran Khalid. A rare case of cardiac paraganglioma presenting as anginal pain: a case report. Cases J. 2009; 2: 72.
- Pradeep K. Yadav, Giselle A. Baquero, Jozef Malysz, John Kelleman, Ian C. Gilchrist. Cardiac Paraganglioma. Circulation: Cardiovascular Interventions. 2014;7:851-856
- Ilias Karabinos, Efthymia Rouska, Nikolaos Charokopos. A primary cardiac paraganglioma. Eur Heart J (2012) 33 (6): 790.
- Hayek ER, Hughes MM, Speakman ED, Miller HJ, Stocker PJ. Cardiac paraganglioma presenting with acute myocardial infarction and stroke. Ann Thorac Surg 2007;83(5):1882–4
- Kennelly R, Aziz R, Toner M, Young V. Right atrial paraganglioma: an unusual primary cardiac tumour. Eur J Cardiothorac Surg. 2008;33:1150–2
- Jebara VA, Uva MS, Farge A, Acar C, Azizi M, Plouin PF, Corvol P, Chachques JC, Dervanian P, Fabiani JN. Cardiac pheochromocytomas. Ann Thorac Surg. 1992;53:356–361.
- Okum EJ, Henry D, Kasirajan V, Deanda A. Cardiac pheochromocytoma. J Thorac Cardiovasc Surg 2005;129(3):674–5.





Comments