ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Repair of Infantile Aortic Coarctation and Transverse Arch Hypoplasia with Resection and Extended End to Undersurface of Aortic Arch Anastomosis
Editors Note
Patient Selection
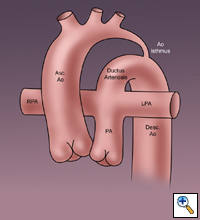
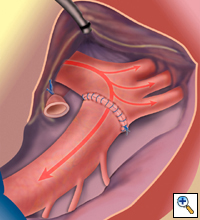
Coarctation of the aorta occurs as a spectrum of disease and comprises approximately 5-8% of all congenital cardiac defects. Infantile coarctation often presents with diffuse tubular hypoplasia of the transverse aortic arch and isthmus with a discrete stenosis where the isthmus inserts into the enlarged ductus arteriosus (Figure1). Hypoplasia of the transverse aortic arch and isthmus is thought to be caused by abnormal fetal blood flow patterns.
Intracardiac lesions that may limit the flow of blood though this area in utero include: ventricular septal defects, and various forms of subvalvar, valvar and supravalvar aortic stenoses as well as various forms of mitral stenosis. The technique of coarctation resection with extended end to undersurface of aortic arch anastomosis addresses the issues of both aortic arch hypoplasia and juxtaductal stenosis.
Anesthesia/Monitoring/Positioning
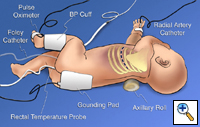
A posterolateral thoracotomy is chosen on the side of the aortic arch. An axillary roll assists with exposure. The third intercostal space gives the best exposure and allows for extended mobilization of the aortic arch. The patient's temperature is monitored with a rectal probe.
Blood pressure cuff and pulse oximeters are placed on the lower extremities. A right radial artery or right axillary artery catheter is used to ensure adequate innominate artery flow and therefore cerebral perfusion following partial occlusion of the aortic arch and ascending aorta. If an umbilical arterial catheter is present, it may be used for measurement of distal aortic pressure following aortic clamping. Towels are placed around the infant to help prevent direct pressure on baby body parts. The rectal temperature is allowed to drift down to the 34-35 degree centigrade range to help with spinal cord and lower body protection during aortic cross clamping.
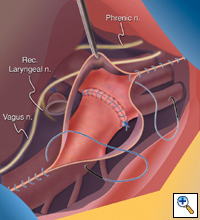
Dissection
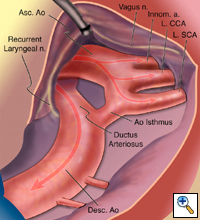
The ascending aorta, transverse aortic arch and its branches, ductus arteriosus and descending aorta must be aggressively mobilized to effect a primary coarctation repair. Care is taken to avoid injury to the recurrent laryngeal which is swept medially out of harms way, and the phrenic nerve which can be quite close in the small infant. Intercostal vessels are mobilized to allow cephalad mobility of the descending aorta and the arch vessels are mobilized to allow caudal mobility of the aortic arch. Lymphatic vessels are controlled with hemoclips
Ductal Ligation
The ductus arteriosus is controlled with two 5-0 Vascufil transfixing sutures. A stay suture is placed in the adventitial layer of the aortic isthmus. A heparin bolus is administered systemically at a dose of 100 units/kg. The ductus is then ligated with the two transfixing sutures.
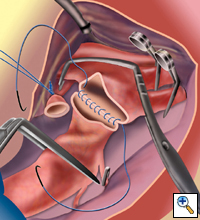
Positioning of Clamps
A Castañeda or similar partial occluding clamp is applied across the entire transverse aortic arch. The clamp is positioned on to the ascending aorta, allowing blood flow through a partially occluded innominate artery. Adequacy of blood pressure is assessed with either a radial or an axillary arterial cannula. Care must be taken to avoid distortion of the innominate artery throughout the repair and close attention is paid to the right radial artery pressure when the clamp is on. The two clamps are held by the same assistant to allow for tension free anastomosis and good exposure. Any small change in position of the proximal clamp can result in inadequate blood flow through the innominate artery. Neurovascular clips are used to occlude backflow from the left carotid and left subclavian artery. Temporary medium titanium hemoclips are used to control intercostal arteries that will not be adequately controlled with an angled aortic cross clamp on the descending aorta. The hemoclips are later removed by squeezing the rounded end with a heavy needle holder. The clamps are stabilized by the first assistant throughout the case. The second assistant will follow the suture used for the anastomosis and keep the field dry with the suction device.
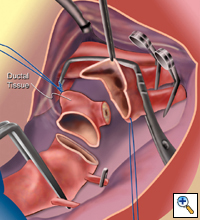
Resection of Ductal Tissue
Once the clamps have been applied, the ductal tissue is excised. The undersurface of the transverse arch is incised proximally on to the ascending aorta and to a position opposite the innominate artery take off. The stay sure placed on aortic isthmus allows splaying open the undersurface of the transverse aortic arch.
Anastomosis
The posterior wall of the anastomosis is done first beginning inside the ascending aorta on the far end. A double loaded 7-0 Vascufil suture on a CV-351 needle is used for this anastomosis. The posterior suture line is continued toward the operating surgeon and it is stopped lateral to the left subclavian artery. The anterior wall of the anastomosis is then completed with the remaining needle. Prior to completion of the anastomosis, the lumen is irrigated with heparinized saline solution. Sodium bicarbonate is administered prior to cross clamp removal.
Completed Anastomosis
The distal clamp is removed first, followed by the proximal clamp and the neurovascular clips that have been applied. Thrombin soaked gel-foam is used to assure hemostasis. Pulse in the distal aorta is checked and the gradient is assessed using umbilical artery or leg pressure measurements.
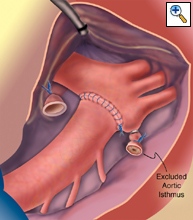
Variation with Exclusion of aortic Isthmus
When the isthmus is long and hypoplastic, anastomosis is made directly to the ascending aorta and arch proximal to the isthmus, which is ligated, to avoid residual obstruction in the transverse arch.
Closure
The parietal pleura is closed over the aorta with a running suture. This is done to create an extra layer should bleeding occur. A single chest tube is left in place.
Closure
The parietal pleura is closed over the aorta with a running suture. This is done to create an extra layer should bleeding occur. A single chest tube is left in place.
Preference Card
Instruments
- Aortic Partial occlusion clamps- Scanlon® Castañeda Clamps
- Aortic cross clamp
- Temporary neurovascular clips- Scanlon® Yasargil-type aneurysm clips
- Medium hemoclips for temporary intercostal artery control
Sutures
- 5-0 Vascufil® on a CV-301 needle for ductal transfixion and ligation
- 7-0 Vascufil® on a CV-351 needle for the aortic anastomosis
Tips & Pitfalls
- Proper positioning. Lateral decubitus slightly leaning back. Axillary roll.
- High thoracotomy in 3rd ICS for best exposure.
- Extensive mobilization of the entire aorta and its branches to avoid tension.
- Place anastomosis as proximal as possible to avoid recurrence.
- Small bites with fine monofilament sutures (7-0) without a lot of tension to avoid stricture or pursestring effect.
Results
Neonatal coarctation with hypoplastic arch can be successfully repaired with resection, mobilization and extended end-to-end anastomosis with low morbidity/mortality and low recurrence rate.
References
- Elgamal MA, McKenzie ED, Fraser CD Jr. Aortic arch advancement: the optimal one-stage approach for surgical management of neonatal coarctation with arch hypoplasia. Ann Thorac Surg 2002;73:1267-1273
- Giamberti A, Pome G, Butera G, Rosti L, Agnetti A, Frigiola A. Extended end-to-end anastomosis with modified reverse subclavian flap angioplasty. Ann Thorac Surg 2001;72:951-2
- Uddin MJ, Haque AE, Salama AL, Uthman BC, Abushaban LA, Shuhaiber HJ. Surgical management of coarctation of the aorta in infants younger than five months: a study of fifty-one patients. Ann Thorac Cardiovasc Surg 2000;6:252-7
- Van Son JA, Mohr FW, Hess H, Hambsch J, Haas GS. Early repair of coarctation of the aorta. Ann Thorac Cardiovasc Surg 1999;5:237-44
- Backer CL, Mavroudis C, Zias EA, Amin Z, Weigel TJ. Repair of coarctation with resection and extended end-to-end anastomosis. Ann Thorac Surg 1998;66:1365-70; discussion 1370-1
- Rajasinghe HA, Reddy VM, van Son JA, Black MD, McElhinney DB, Brook MM, Hanley FL. Coarctation repair using end-to-side anastomosis of descending aorta to proximal aortic arch. Ann Thorac Surg 1996;61:840-4