ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Retroverted Left Atrial Appendage: A Previously Undescribed Variant
Chia RH (Misté), Joshi P. Retroverted Left Atrial Appendage: A Previously Undescribed Variant. July 2024. doi:10.25373/ctsnet.26381620
Introduction
As the main source of cardiogenic emboli, left atrial appendage (LAA), accounts for more than 90 percent of embolic strokes (1, 2). It has been referred to as the most “lethal human attachment” (2). Various shapes, namely cactus, chicken wing, windsock, and cauliflower, have been described in the literature (3). These descriptions, however, have not detailed the location of the appendage tip, since its location does not bring about significant implications during insertion of intracardiac devices. In a majority of cases, the tip of the LAA is located lateral to the pulmonary artery (PA), though the exact incidence of such occurrence has not been studied. The unobscured view of the appendage tip in an anteverted LAA facilitates relatively easy access when passing an extracardiac device during thoracoscopic occlusion. With increased popularity in the application of extracardiac devices for LAA occlusion, the authors came across a previously undescribed anatomical variation, a retroverted LAA.
LAA Anatomy and Implications During Thoracoscopic Occlusion
Retroverted LAA is not a widely recognized anatomical variant and its incidence has not been reported. Unlike an anteverted LAA, its tip is not in its usual location (lateral to the PA) and is, therefore, not readily visible endoscopically (Figures 1A, B). This is because it runs in the transverse sinus, which is posterior to the right ventricular outflow tract, PA, and aorta (Figures 1C, D). The base or neck of the LAA remains unchanged.
Cardiac computed tomography with contrast enhancement is very reliable in identifying a retroverted LAA preoperatively (Figures 1C, D). Magnetic resonance imaging is as useful, especially in patients with contraindication to contrast. Transesophageal echocardiography, which is routinely performed to assess for LAA thrombus preoperatively, can help identify a retroverted appendage.
It is essential to visualize the appendageal tip to allow deployment of the occlusion device to sit at the appendageal base. Intraoperative maneuvers can help optimize device sitting and are highlighted in the video.
Conclusion
Retroverted LAA is an underrecognized anatomical entity. Its tip runs in the transverse sinus and is not readily visible. This video showcases surgical steps for optimal extracardiac device placement.
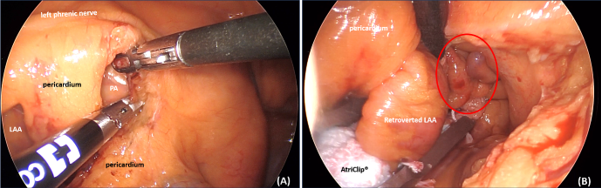

Figure 1
Figure 1A, B. A and B are endoscopic views of the mediastinum: A illustrates the close relationship of the pericardiotomy site to important structures such as the left phrenic nerve and PA. B demonstrates the examination of atrioventricular groove (with the red circle highlighting the medial lobe of a retroverted LAA, which can easily be missed during thoracoscopic LAA occlusion. Figure 1C, D.
C and D are axial and sagittal CT images, respectively, showing a retroverted LAA lying posterior to the RVOT, PA and aorta; CT, computed tomography; LAA, left atrial appendage; PA, pulmonary artery; RVOT, right ventricular outflow tract; and SVC, superior vena cava.
References
- Blackshear JL, Odell JA. Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann Thorac Surg. 1996;61(2):755-9.
- Johnson WD, Ganjoo AK, Stone CD, et al. The left atrial appendage: our most lethal human attachment! Surgical implications. Eur J Cardiothorac Surg. 2000;17:718-22.
- Di Biase L, Santangeli P, Anselmino M, et al. Does the Left Atrial Appendage Morphology Correlate With the Risk of Stroke in Patients With Atrial Fibrillation?:Results From a Multicenter Study. 2012;60(6):531-8.
Disclaimer
The information and views presented on CTSNet.org represent the views of the authors and contributors of the material and not of CTSNet. Please review our full disclaimer page here.




Comments