ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Trans-Subxiphoid Robotic-Assisted Thymectomy
Calderoni M, Ceruti E, Ferrari M, Pardolesi A. Trans-Subxiphoid Robotic-Assisted Thymectomy. September 2024. doi:10.25373/ctsnet.26928625
Median sternotomy has been the most commonly used approach for thymectomy to date. Recent advances in video-assisted thoracoscopic surgery (VATS) and robotic-assisted techniques with CO2 insufflation have allowed more minimally invasive approaches. Subxiphoid thymectomy is a well-known procedure, and its incision provides excellent exposure for surgeons and results in reduced postoperative pain. Thymectomy in block with mediastinal fat was the procedure of choice for every suspected anterior mediastinal lesions suggestive of thymoma.
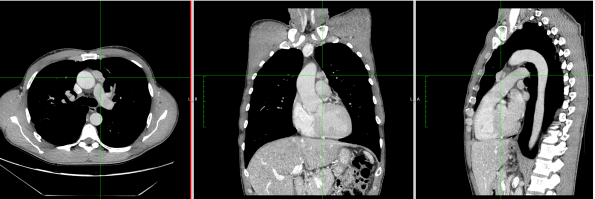

1. CT-Scan and PET-Scan
Preference Cards:
- 30-degree 10 mm robotic camera
- Co2 Insufflation device (8-10 mmHg)
- Tissue retractor: GelPort (Applied Medical), robotic trocars
- 8 mm robotic instruments (EndoWrist bipolar Maryland, Fenestrated bipolar forceps, Synhroseal)
- Endoscopic retrieval bag
Clinical Vignette:
A 47-year-old male patient with no previous medical history was referred to the institution with a diagnosis of mediastinal mass suspected of being thymoma, without any clinical or laboratory signs of myasthenia gravis. The chest CT-scan showed a 2.5 cm lesion with no clear signs of infiltration of surrounding tissues and with a PET uptake of SUV max 4. The patient was scheduled for subxiphoid bilateral robotic-assisted thymectomy.
Surgical Technique:
The surgeons performed a 3 cm subxiphoid incision. A GelPort (S) was placed, and CO2 was insufflated with pressure from 8 to 10mmHg. The camera port was introduced through the GelPort in the subxiphoid area. Under direct view, the surgeons introduced an operative port in the seventh right intercostal space on the anterior axillary line. Then, the second operative port was placed in the contralateral intercostal space, again at the level of the anterior axillary line. The docking required less than four minutes. A fenestrated bipolar forceps was introduced through the right port, and the bipolar Maryland was introduced in the left chest cavity.

2: Graphic Representation of Port Placement and Patient Disposal
The procedure started by dividing the tissue beneath the sternum from the lower to the upper edge of the manubrium. This maneuver, combined with CO2 inflation, created a large operative space with anatomical landmarks that could be easily identified: the left and right internal arteries and the left and right phrenic nerves. The surgeons continued by dividing the lower thymic horns. Using the Syncrosyl, the surgeons safely divided large arteries and veins that supplied blood to the mediastinal fat tissue. Dissection was continued, separating the fat tissue from the pericardium plane in an upward direction, exposing the ascending aorta and the superior cava vein.
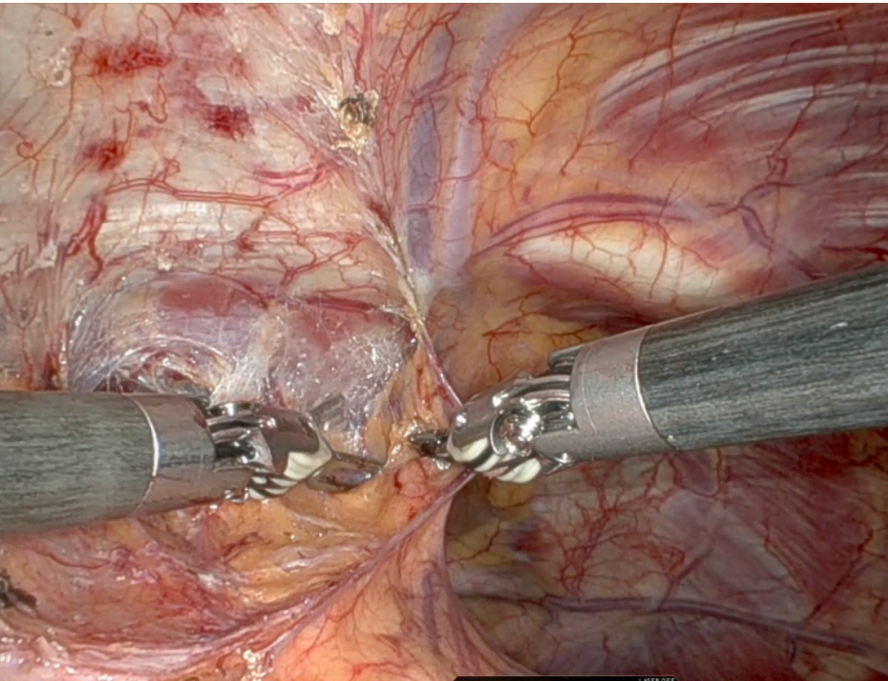
Adhesions with lung parenchyma can be divided with bipolar Maryland or Syncrosyl as well. In this case, there were no signs of lung parenchyma infiltration; otherwise, the surgeons would have performed a wedge resection of the lung.
The tumor was located on the left side of the mediastinum, tenaciously adherent to the phrenic bundle. However, there was no direct infiltration of the nerve, and the surgeons were able to carefully dissect and preserve the nerve along its length across the left mediastinal side.
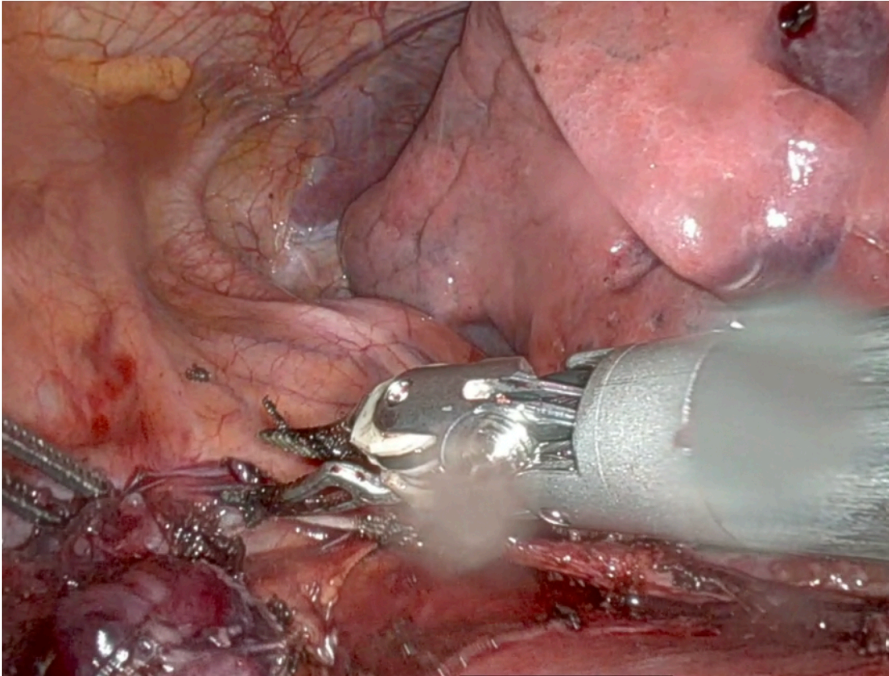
After dissecting the fat tissue from the right phrenic nerve, the surgeons proceeded to dissect the mediastinal tissue from the cava vein until they encountered the anonymous vein. Once the anonymous vein was identified, the surgeons dissected the upper horns, stripping the fat tissue from the lower part of the neck. The thymic vein was safely divided with Syncrosyl without the need for clips or Hem-o-lok. The specimen was extracted safely
to avoid tumors from spreading, using an endobag introduced from the subxiphoid access. The subxiphoid approach allowed for an accurate and oncologically valid dissection of all the mediastinal fat tissue en bloc with the tumor.
Tips and Tricks:
The subxiphoid access, combined with CO2 inflation, created a large operative space in the anterior part of the mediastinum and allowed for safe dissection at the thoracic inlet, with all vascular structures and nerves always under direct control.
When performing an extended thymectomy, it is mandatory to dissect all the anterior mediastinal fat from phrenic to phrenic, as oncological criteria suggest. Sometimes the lesion can present a close extension to the phrenic nerve path. Preserving the nerve is fundamental to avoid any postoperative immediate and long-term complications (e.g., paralysis, diaphragmatic relaxation, respiratory failure).
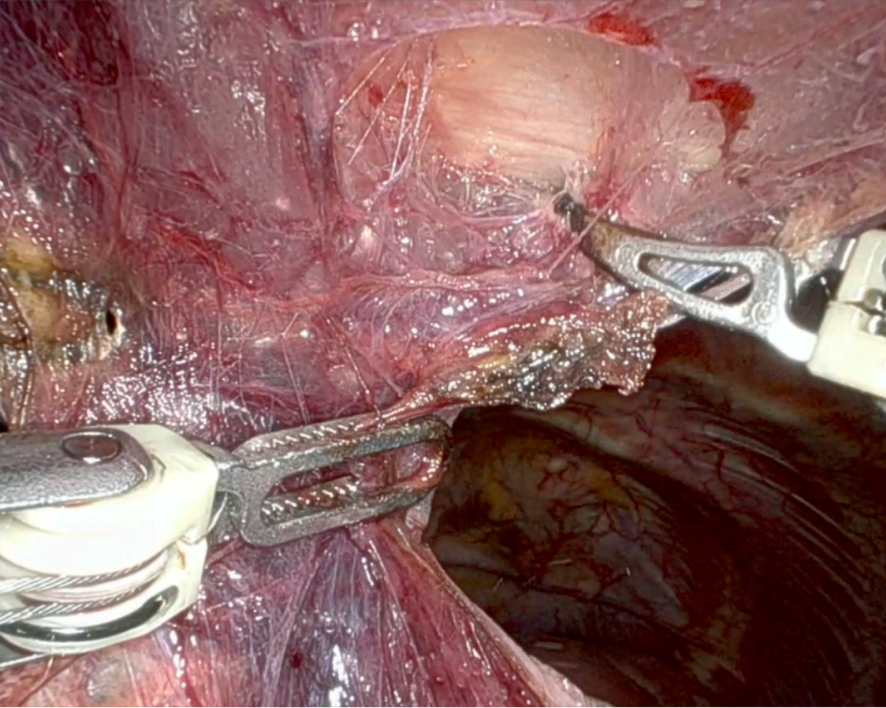
2A: Substernal Dissection
2B: Complete Exposure of Mediastinal Artery and Veins
2C: Safe Phrenic Dissection
Conclusion
The trans-subxiphoid robotic thymectomy is a valid option even for extended thymectomy. Its large view allows surgeons to perform the mediastinal dissection safely and easily, while preserving all oncological criteria.
References
- Katie E. O’Sullivan, Usha S. Kreaden, April E. Hebert, Donna Eaton, Karen C. Redmond Ann Cardiothorac Surg. 2019 Mar; 8(2): 174–193. doi: 10.21037/acs.2019.02.04
- Diego Gonzalez-Rivas, Mahmoud Ismail J Thorac Dis. 2019 Jan; 11(1): 231–239. doi: 10.21037/jtd.2018.12.94
Disclaimer
The information and views presented on CTSNet.org represent the views of the authors and contributors of the material and not of CTSNet. Please review our full disclaimer page here.




